Why Sulfa-Free Antibiotics Matter in 2025
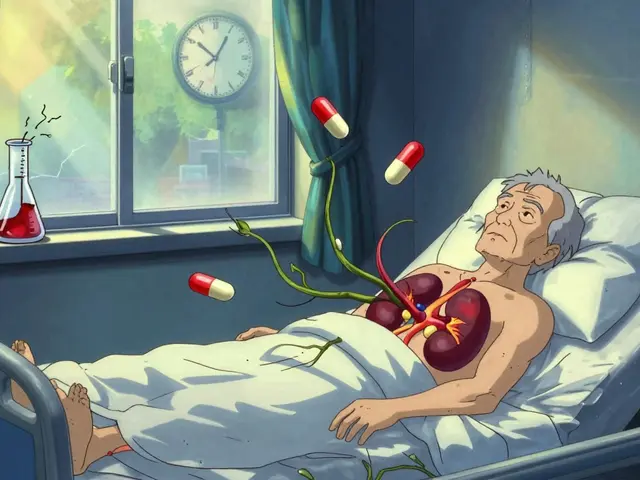
Sulfa drugs—those classic antibiotics with the 'sulfa' label—have been game-changers since the ’30s. But for some folks, these meds can lead to more problems than they fix: think hives, fever, severe rashes, or even life-threatening reactions like Stevens-Johnson Syndrome. About 3% of the population deals with some allergic response to sulfonamides. Does that sound rare? Around 30 million antibiotic prescriptions are written every year in North America, so that allergy still affects a ton of people. And it’s not just about allergies; some sulfa drugs can mess with folks who have certain health conditions—like those with kidney problems or G6PD deficiency.
These days, the antibiotics world is more complex than ever. As doctors get stricter about prescribing, patients with allergies shouldn’t have to gamble with their health. That’s why knowing which antibiotics are truly sulfa-free is a bigger deal than most people realize. Not all antibiotics with a similar-sounding name or structure will set off an allergy, but there’s still confusion, especially in local pharmacies or small clinics. Take it from someone who’s seen the inside of a clinic—mistakes happen more than you’d think. Plus, as more bugs become resistant to the big, broad-spectrum meds, having safe alternatives is like gold dust.
Let’s clear up a big myth: just because a drug has sulfur in its makeup (like some pain meds, diuretics, or diabetes drugs) doesn’t mean it’s a 'sulfa antibiotic.' We’re talking about sulfonamide antibiotics, with the best-known examples being sulfamethoxazole and sulfasalazine. You’ll find sulfamethoxazole paired with trimethoprim in Bactrim, one of the most common first-line antibiotics for everything from urinary tract infections to MRSA skin infections. But if that’s off the table, a whole new path opens up for choosing the right treatment, and it’s not one-size-fits-all.

The Top Sulfa-Free Antibiotics and When They’re Used
The universe of sulfa-free antibiotics is huge now, with different families offering unique pros and cons. Let’s break it down into practical choices, focusing on what works for real people—not just textbook cases.
- Penicillins (like amoxicillin or penicillin V): Old school, but still reliable for strep throat, ear infections, and a bunch of basic bacterial issues. A lot of people worry about cross-allergy between penicillins and sulfas, but they’re actually unrelated. If you’ve reacted to sulfa drugs, you can usually use penicillins, unless you’re also allergic to that class—which is a whole other story.
- Cephalosporins (cephalexin, cefdinir, cefuroxime): These meds knock out respiratory infections, UTIs, skin wounds, and more. The risk of allergic cross-reaction with sulfa antibiotics is close to zero—they’re totally different animals.
- Macrolides (azithromycin, clarithromycin, erythromycin): Go-to choices for respiratory bugs, sinus infections, and even some nasty skin infections. They’re especially handy for folks who can’t take penicillins for any reason.
- Tetracyclines (doxycycline, minocycline): These antibiotics punch above their weight, handling acne, chlamydia, tick-borne Lyme disease, and pneumonia. Doxycycline, in particular, pops up in guidelines all over the place because bacteria haven’t figured out how to defeat it as much—yet.
- Fluoroquinolones (ciprofloxacin, levofloxacin, moxifloxacin): These workhorses used to be more common, but now doctors use them when others fail, thanks to potential side effects. Still, they handle tough urinary or GI infections with no sulfa in sight.
- Clindamycin: Often the best ticket for skin abscesses, dental infections, and bone or joint problems where other options won’t work. It’s completely unrelated to sulfa antibiotics and even covers some MRSA strains—something Bactrim usually gets credit for.
Here’s where things get interesting. No one antibiotic is 'the best'—it depends on your infection, your age, the bacteria involved, and your medical history. For example, nitrofurantoin is a solid, targeted urinary tract infection treatment, but it’s almost useless for lung infections. Doxycycline’s a star for skin and certain tick illnesses but won’t fix a bladder infection reliably in men. The right fit depends on the bug and the body part, not just the label.
What about effectiveness? Modern studies compare these drugs head-to-head all the time. In a 2024 head-to-head trial, cephalexin treated complicated skin infections (those usually handled by Bactrim) with similar cure rates and fewer side effects. Regular old penicillin is still top dog for group A strep—something the Bactrim combo can’t reliably kill. And while azithromycin gets handed out like candy for coughs, its real strength is in lung or sinus infections where resistance rates are still low.
One mistake I see people make: grabbing the nearest non-sulfa antibiotic without checking if it even works for their specific infection. If you’ve got a urine infection, clindamycin won’t help. For pneumonia, nitrofurantoin is useless. It pays—literally—to know the matchups for each drug, infection, and allergy risk.
Looking for more options? You can even find a detailed guide comparing each Bactrim alternative for 2025 treatment landscapes, breaking down which works best for which infections and sensitivity patterns.

Navigating Allergies, Resistance, and Real-Life Choices with Sulfa-Free Antibiotics
Real talk: if you’ve ever had a bad reaction to sulfa antibiotics, you know that quick answer—just pick something else—isn’t always that simple. Not every doctor is on top of the latest guidelines, and not every clinic can test your exact bacterial strain. Navigating these choices means knowing not only which drugs are safe, but which will actually do the job against common modern bugs.
Start with the basics: tell your provider about your allergy details. Was it a mild itch, or a full-body rash with trouble breathing? Knowing how severe things got points doctors toward the safest and most effective backup. Don’t just say 'allergic to sulfur.' Lots of people confuse sulfa antibiotics with other sulfur-containing drugs and miss out on treatments they could actually take.
Keep a medication allergy list handy—on your phone, wallet, or an emergency medical card. If you’re prone to allergic disasters like me, having this info ready can actually influence which drugs an ER doctor grabs in an emergency. For my wife, Elara, who once got a massive rash from Bactrim, we keep a printout in our glove box and digital docs stored on our phones. It’s come in handy more than once while traveling.
Here’s a pro tip: some infections now need a culture—a test to check exactly which bacteria are causing trouble and what drugs they’re sensitive to. This can add a day or two to getting a prescription, but it saves you from cycling through weak or unsafe antibiotics. In 2025, many urban clinics have switched to this model for urine and wound infections because resistance patterns are shifting so fast.
Wondering how resistant bacteria have become? Here’s a real-world peek:
| Antibiotic | Percent Resistance – E. coli (UTI) |
|---|---|
| Amoxicillin | 36% |
| Nitrofurantoin | 2% |
| Ciprofloxacin | 21% |
| Sulfamethoxazole/Trimethoprim | 18% |
Resistance rates like those change every year, so always check if your infection is covered by the drug your doctor picks—and if you need a backup. The good news for the sulfa-free crowd? Nitrofurantoin and most cephalosporins are still holding strong in the resistance wars, especially for bladder bugs.
If you’re considering a Bactrim alternative, ask pharmacists about the latest resistance data in your area. It can be very local—sometimes one side of a city will show much higher rates for a certain bug than the other. Don't be shy: pharmacists often know more about what’s working in town than doctors do, since they see all the scripts for the week.
Another tip: don’t hesitate to request non-sulfa drugs for preventive uses if you’re at risk—like after some dental procedures, or before travel to malaria-risk zones. Doxycycline can be used instead of sulfa meds for malaria, and azithromycin is used for traveler’s diarrhea without the allergy worry. If you’re heading into surgery or dealing with repeated infections, your healthcare team can find the right non-sulfa med for the situation.
Finally, advocate for yourself. Doctors see hundreds of patients a week, and it’s easy for details like a past medication allergy to slip through the cracks. Label allergies in every chart, every urgent care app, and every pharmacy file. If you experience anything weird—like a new rash or shortness of breath after starting something—call the prescriber right away. It’s safer to sound fussy than to face an ER visit.
2025 is all about smart, safe infection fighters. Sulfa-free antibiotics are everywhere—you just have to know your story, speak up, and make sure the drug matches the bug you’re fighting. The right alternative is out there, and with the tools above, there’s no reason to gamble with your health again.