Every day, pharmacists make decisions that can mean the difference between effective treatment and serious harm. One of the most high-stakes areas? Generics. With 90% of prescriptions filled with generic drugs in the U.S., and new approvals rising by 17% year over year, staying sharp on generics isn’t optional-it’s essential. But the rules change fast. The FDA updates therapeutic equivalence ratings monthly. States tweak substitution laws. Biosimilars now require their own set of rules. And if you get it wrong? You’re not just risking a patient’s health-you’re risking your license.
Why Generics Education Isn’t Just Another Box to Check
Most pharmacists complete their required continuing education (CPE) to renew their license. But too many treat it like a chore. That’s dangerous. In 2021, ACPE found that 42.7% of all pharmacy malpractice claims involved errors with generic substitution. That’s not a small number. That’s nearly half of all legal issues tied to medication errors.
Why does this happen? Because generics aren’t just cheaper versions of brand-name drugs. They’re complex products with strict regulatory standards. The FDA requires generics to match brand-name drugs in identity, strength, purity, and quality. But more importantly, they must demonstrate bioequivalence-meaning the drug gets into the bloodstream at the same rate and extent as the original, within an 80-125% range. That’s not just theory. That’s daily practice.
Take levothyroxine. It’s one of the most commonly prescribed drugs in the U.S. But even small differences in bioavailability between generic brands can cause thyroid levels to swing dangerously. A pharmacist who doesn’t know the Orange Book’s therapeutic equivalence codes (like AB1, AB2, BX) could accidentally swap two products that aren’t interchangeable. One pharmacist in Illinois told me she caught a dangerous substitution last year because of a CE module she took on therapeutic equivalence. She didn’t just avoid a mistake-she prevented a hospital visit.
What You Need to Know: The Core Topics
To stay compliant and safe, your continuing education must cover these five areas:
- The FDA Orange Book - This is your bible. It lists approved generic drugs and their therapeutic equivalence ratings. You need to know how to read it. AB-rated means substitutable. BX means not recommended for substitution. These codes change monthly. If you’re not checking them regularly, you’re working blind.
- Abbreviated New Drug Applications (ANDAs) - This is how generics get approved. Understanding the ANDA process helps you see why some generics are more reliable than others. The FDA requires bioequivalence studies, but not all manufacturers follow the same standards. Some use different inactive ingredients that can affect absorption.
- State Substitution Laws - Not all states are the same. Texas has strict rules for narrow therapeutic index (NTI) drugs like warfarin or phenytoin. California requires pharmacists to notify patients when substituting. New York mandates documentation. Illinois doesn’t require proof unless audited. Know your state’s rules-or you could be violating the law.
- Biosimilars and Interchangeability - These aren’t traditional generics. Biosimilars are complex biologic drugs with no exact copy. The FDA has a separate designation for “interchangeable” biosimilars. Only those can be substituted without prescriber approval. In 2023, 78% of hospital pharmacists said they needed more training here. If you’re working in a hospital or clinic, this isn’t optional anymore.
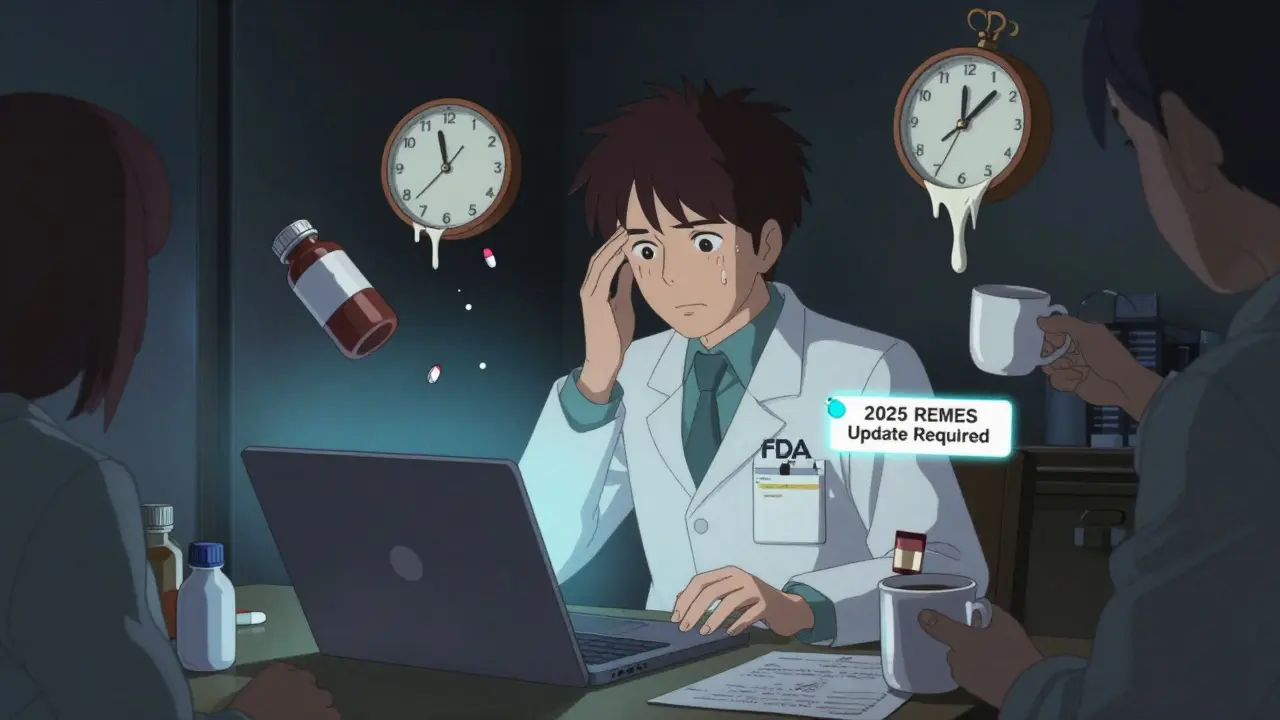
- Legal and Ethical Pitfalls - The CREATES Act was passed to stop brand-name companies from blocking generic manufacturers from getting samples. But it’s created new legal gray areas. Pharmacists can’t assume a generic is safe just because it’s on the market. If a manufacturer is under litigation or has a REMS program (Risk Evaluation and Mitigation Strategy), you need to know it. Ignorance isn’t a defense.
How to Choose the Right CE Courses
Not all continuing education is created equal. You’ve probably taken those 1-hour online modules that feel like watching a PowerPoint with voiceover. They’re boring. And worse-they don’t stick.
Look for courses that are:
- ACPE-accredited - Only these count toward your license renewal. State boards don’t accept random webinars.
- Application-based - These use real case studies. One course might walk you through a patient on warfarin who had a spike in INR after switching generics. You analyze the lab results, check the Orange Book, and decide what to do. These courses get 4.7/5 stars on CE21. Knowledge-based ones? 3.2/5.
- State-specific - If you practice in multiple states, find courses that break down differences. Texas and California have very different substitution rules. Don’t assume what works in one state applies to another.
- Updated for 2025 - Starting January 1, 2025, ACPE will require all generics-related CE to include content on biosimilar interchangeability and FDA REMS programs. If your course doesn’t mention these, it’s outdated.
Free options exist. Pharmacist’s Letter offers accredited modules on therapeutic equivalence and ethics at no cost. But don’t just take the free ones because they’re cheap. Take the ones that challenge you.

Real-World Challenges Pharmacists Face
Here’s what actually happens in pharmacies:
- A patient gets a refill on a generic statin. The pharmacy system auto-substitutes it with a different generic. The patient comes back two weeks later with muscle pain. Turns out the new generic had a different filler that affected absorption.
- A nurse calls asking if they can substitute a biosimilar for a biologic. The pharmacist says yes-without checking if it’s FDA-designated as interchangeable. That’s a liability.
- A pharmacist in Florida fills a prescription for a generic antidepressant. The patient reports it’s not working. The pharmacist checks the Orange Book and realizes the brand and generic are AB-rated, but the patient had been on a specific manufacturer’s version for years. The pharmacist calls the prescriber to ask if they want to stick with that brand.
These aren’t hypotheticals. They’re daily realities. And they all come down to one thing: knowledge gaps.
A 2022 APhA survey found pharmacists who completed at least 5 hours of generics-specific CE annually made 37% fewer substitution errors. That’s not a small improvement. That’s life-changing.
How Much Time Should You Really Spend?
The average pharmacist spends 27.5 hours a year on CE. But only 5.2 of those hours are focused on generics and therapeutics. That’s not enough.
Experienced pharmacists-those with 10+ years in practice-need 8 to 10 hours a year just on generics. Why? Because the field moves faster than you think. New drugs, new regulations, new lawsuits. You can’t rely on what you learned in pharmacy school.
Newer pharmacists might think they’re up to date. But even they need 4 to 6 hours of targeted training. The landscape changed dramatically between 2020 and 2025. If your last generics course was before 2022, you’re already behind.
And don’t forget state requirements. Illinois now requires 1 hour of Cultural Competency training starting in 2025. Other states mandate sexual harassment prevention or implicit bias training. You can’t afford to miss those either.
What’s Changing in 2025 and Beyond
The rules are tightening. Here’s what’s coming:
- ACPE’s 2025 standards - All generics CE must now include biosimilar interchangeability and REMS content. If your provider hasn’t updated their courses, they’re not compliant.
- NABP’s push for standardization - Right now, 18 states require opioid alternative training, 12 require biosimilar education, and 7 have special rules for NTI drugs. The National Association of Boards of Pharmacy wants 80% of states to align by 2025. That’s good news-but until then, you still need to know each state’s rules.
- AI-powered learning - Platforms like PocketPrep are using AI to identify your weak spots. If you keep missing questions on therapeutic equivalence, the system flags it and pushes targeted content. Early adopters report better retention and fewer errors.
- Point-of-care tools - CVS Health piloted a system that gives pharmacists real-time alerts when a substitution might be risky. The result? A 28% drop in generics-related errors. This isn’t science fiction-it’s happening now.
The future of pharmacy isn’t just about dispensing pills. It’s about making smart, evidence-based decisions in real time. And that requires ongoing learning-not just to stay licensed, but to stay safe.
What to Do Next
Here’s your action plan:
- Check your state’s CE requirements. Don’t guess. Go to your board of pharmacy’s website.
- Review your last 2 years of CE. Did any of it focus on therapeutic equivalence, biosimilars, or state substitution laws?
- Find at least two ACPE-accredited, application-based courses for 2025. Prioritize ones that include case studies.
- Bookmark the FDA Orange Book. Check it once a month.
- Join a peer group or online forum. Talk to other pharmacists about recent substitution issues. You’ll learn more from real stories than any lecture.
Generics are the backbone of modern pharmacy. But they’re also the most misunderstood. If you’re not actively learning about them, you’re not just falling behind-you’re putting patients at risk. The next time you fill a prescription for a generic drug, ask yourself: Do I really know what I’m giving? If the answer isn’t a confident yes, it’s time to learn.
Do all states require the same continuing education for pharmacists on generics?
No. While all 50 states require continuing education for license renewal, the specific requirements vary. Some states mandate hours on biosimilars, narrow therapeutic index drugs, or opioid alternatives. Others require cultural competency or implicit bias training. For example, Illinois requires 30 hours every two years, including 1 hour of Cultural Competency training starting in 2025. Texas has strict rules for substituting generic versions of drugs like warfarin. Always check your state board’s official website for current requirements.
What is the FDA Orange Book and why does it matter for pharmacists?
The FDA Orange Book is the official publication listing approved generic drugs and their therapeutic equivalence ratings. It uses codes like AB (substitutable) and BX (not recommended for substitution). Pharmacists rely on it daily to determine whether a generic can be safely swapped for a brand-name drug. Ratings are updated monthly, so checking it regularly is critical to avoid substitution errors that could harm patients.
Are biosimilars the same as generic drugs?
No. Biosimilars are highly similar to biologic drugs (like Humira or Enbrel), but they’re not exact copies because biologics are made from living cells. Generic drugs are exact copies of small-molecule drugs like metformin or lisinopril. Only biosimilars designated as “interchangeable” by the FDA can be substituted without prescriber approval. Many pharmacists lack training on this distinction, leading to confusion and potential errors.
How many hours of CE should I dedicate to generics each year?
At minimum, aim for 5-6 hours per year. For pharmacists with 10+ years of experience, 8-10 hours is recommended due to the rapid pace of change. The average pharmacist only spends 5.2 hours annually on generics-specific education, but studies show those who invest more make 37% fewer substitution errors. Prioritize application-based courses with case studies-they’re more effective than passive lectures.
Can I use free CE courses to meet my state’s requirements?
Yes-if they’re accredited by ACPE or your state board of pharmacy. Free courses from Pharmacist’s Letter, for example, are ACPE-accredited and cover key generics topics like therapeutic equivalence and ethics. But avoid free webinars or YouTube videos unless they’re officially accredited. Unaccredited courses won’t count toward license renewal and could leave you non-compliant.