For people living with moderate to severe COPD, frequent flare-ups - or exacerbations - can mean hospital visits, lost days at work, and a steady decline in quality of life. The good news? A targeted treatment called triple inhaler therapy has shown real, measurable benefits for the right patients. But it’s not a one-size-fits-all solution. Understanding who benefits, how it works, and what the risks are can make all the difference.
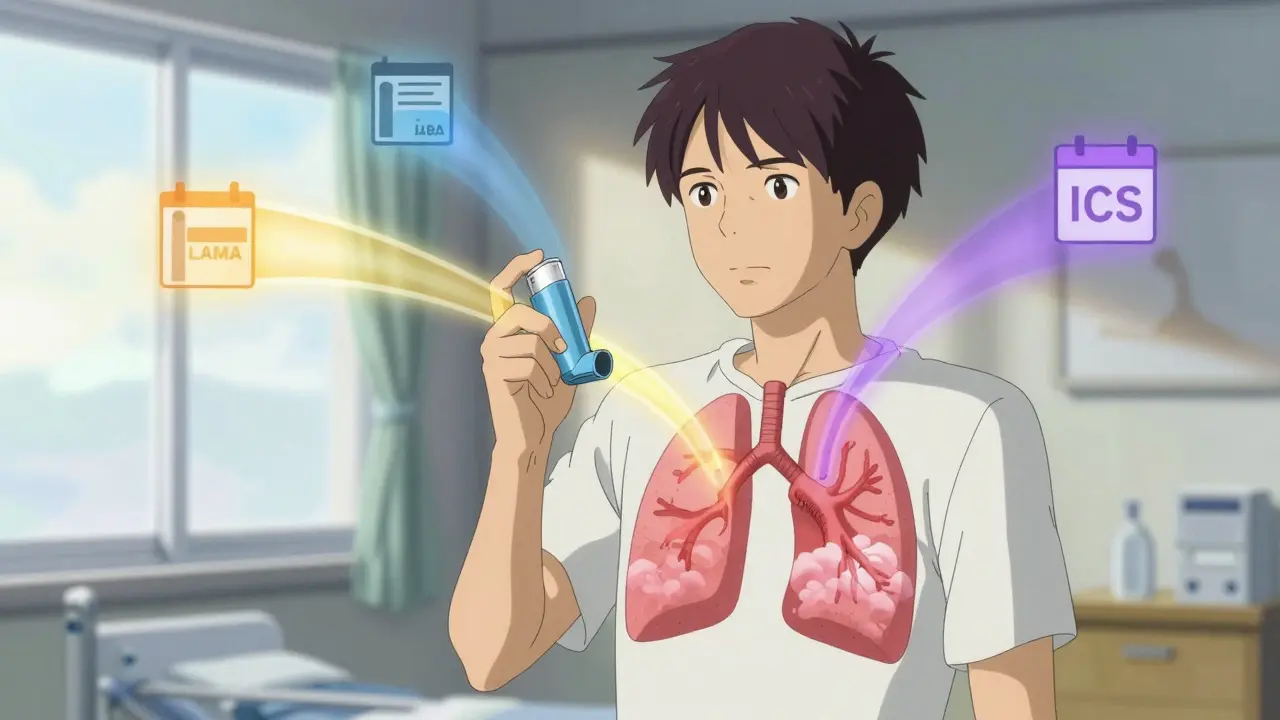
What Is Triple Inhaler Therapy?
Triple inhaler therapy combines three types of medications in one regimen: an inhaled corticosteroid (ICS), a long-acting muscarinic antagonist (LAMA), and a long-acting beta-agonist (LABA). Each plays a different role. The LAMA relaxes the airway muscles, the LABA opens them further, and the ICS reduces inflammation in the lungs. Together, they tackle the three main problems in COPD: narrowed airways, excess mucus, and chronic swelling.There are two ways to take this combo. One is using three separate inhalers - known as multiple-inhaler triple therapy (MITT). The other is a single device that delivers all three drugs at once - called single-inhaler triple therapy (SITT). Devices like Trelegy Ellipta (fluticasone furoate/umeclidinium/vilanterol) and Trimbow (budesonide/glycopyrronium/formoterol) are the most common SITT options. They’re designed to simplify treatment: one puff, once or twice a day, instead of juggling multiple devices.
Who Benefits Most From Triple Therapy?
Not everyone with COPD needs or should use triple therapy. According to the 2024 GOLD guidelines, it’s recommended only for patients who meet two clear criteria:- They’ve had at least two moderate exacerbations in the past year, or one severe exacerbation that required hospitalization.
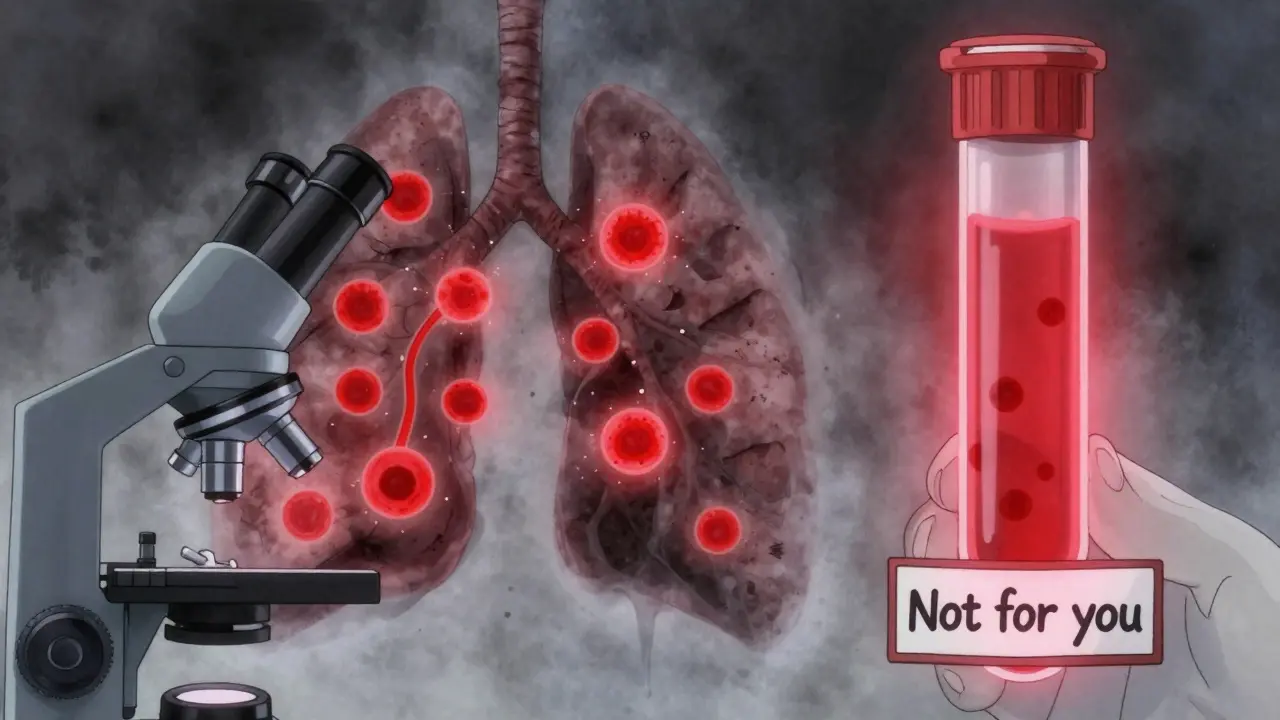
- They have blood eosinophil counts of 300 cells/µL or higher.
Eosinophils are a type of white blood cell linked to airway inflammation. When these numbers are high, it signals that inflammation is a major driver of their COPD - and that’s exactly where the ICS component works best. Studies like IMPACT and ETHOS showed that in this group, triple therapy can reduce moderate-to-severe exacerbations by about 25% compared to dual therapy (LAMA/LABA alone).
But if your eosinophil count is below 100 cells/µL, triple therapy offers little to no benefit - and may actually increase your risk of pneumonia. In fact, fluticasone-based triple inhalers have been linked to a 1.83-fold higher pneumonia risk than budesonide-based ones. That’s why doctors now test eosinophil levels before prescribing this treatment.
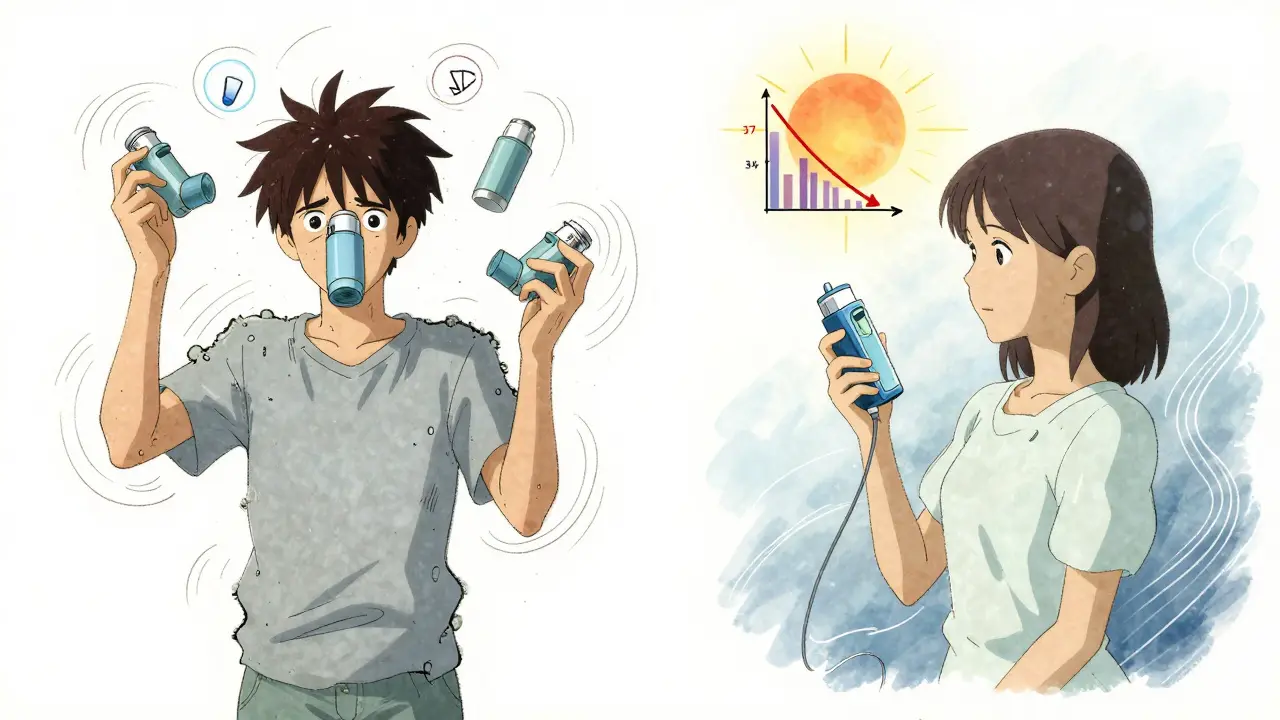
SITT vs MITT: Adherence Makes All the Difference
Using three separate inhalers sounds simple - until you forget which one does what, or leave one at home. Real-world data from the TARGET study found that only 62.1% of patients stuck with MITT after 12 months. The top reasons? Forgetting doses (42.7%) and confusion about the routine (29.3%).Switching to a single-inhaler device changed that. Adherence jumped to 78.4% with SITT. In one study of patients who switched from MITT to SITT, exacerbations dropped by 37% in just six months. Why? Because simplicity works. One device. One routine. Less to manage. Patients in the TRINITY study said the biggest advantage was having “less equipment to carry” and a “simpler daily routine.”
But it’s not just about convenience. SITT also ensures you get the full dose of all three drugs together. With MITT, inconsistent timing or technique can mean one component is under-dosed - reducing the overall benefit.
The Controversy: Is the Benefit Real?
There’s debate in the medical community. Some experts point to randomized trials like IMPACT and ETHOS, which showed clear reductions in exacerbations. Others argue those studies may have exaggerated the benefit.Dr. John Blakey and others suggest that in many of these trials, patients were switched from triple therapy to dual therapy - meaning the “control” group was actually being taken off a drug they were already on. This “washout effect” may have made dual therapy look worse than it really is. When real-world data from the UK (analyzing 31,000 patients) looked at people who stayed on their original treatment, the difference between triple and dual therapy vanished.
The FDA and EMA both rejected claims that triple therapy reduces mortality. And while GOLD 2024 still recommends it for high-risk, eosinophil-high patients, they emphasize it’s not for everyone. As Professor Dave Singh put it: “Triple therapy should be reserved for patients with specific phenotypic characteristics.”
Practical Challenges: Cost, Technique, and Monitoring
Even if you’re the right candidate, using triple therapy isn’t always straightforward.Cost is a major barrier. In the U.S., brand-name SITT inhalers like Trelegy Ellipta can cost $75-$150 per month out-of-pocket. A 2022 study found that 22.3% of Medicare beneficiaries skipped doses because they couldn’t afford them. Generic alternatives are still limited, and insurance coverage varies widely.
Inhaler technique matters more than you think. Studies show 50-70% of patients who seem to “not respond” to treatment actually just don’t use the device correctly. Devices like the Ellipta require specific breathing patterns - inhale deeply, hold your breath, then exhale slowly. A single training session isn’t enough. Clinicians now use checklists to verify technique at every visit.
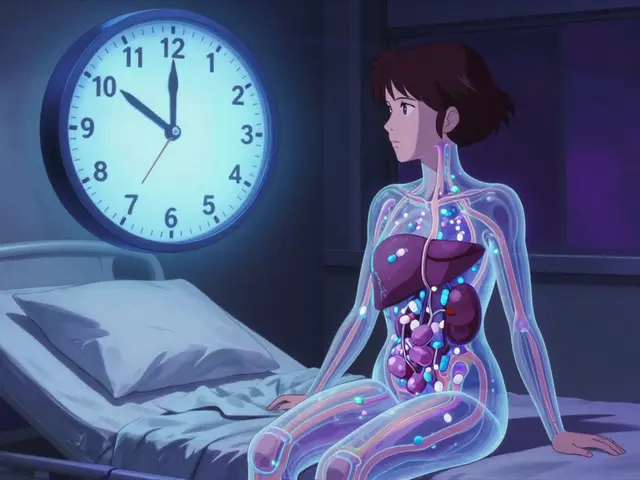
Monitoring is essential. Doctors should check blood eosinophil levels before starting and again every 6-12 months. Spirometry (lung function tests) should be done quarterly. And patients must be alert for signs of pneumonia - fever, increased mucus, worsening shortness of breath - because ICS use increases this risk.
What’s Next? The Future of COPD Treatment
The field is moving toward precision medicine. Researchers are testing whether other biomarkers - like fractional exhaled nitric oxide (FeNO) - can predict ICS response better than eosinophils. The EXACT study is currently exploring this.Meanwhile, new biologics like dupilumab are showing promise in phase 3 trials for COPD patients with high eosinophils. These injectable drugs target specific inflammatory pathways and may eventually replace ICS in some cases - with fewer pneumonia risks.
By 2027, experts predict biomarker-guided therapy will become standard. That means your treatment won’t be chosen based on your diagnosis alone - but on your unique biology. For now, triple inhaler therapy remains a powerful tool - but only for those who fit the profile.
Bottom Line
Triple inhaler therapy isn’t a cure. It’s a targeted tool. If you’ve had multiple COPD flare-ups and your blood test shows high eosinophils, it can cut your risk of hospitalization. If you’re on three inhalers and struggling to keep up, switching to a single device might improve your adherence and reduce flare-ups. But if your eosinophils are low, or you’re not having frequent exacerbations, triple therapy won’t help - and could hurt.Ask your doctor: “Do I meet the criteria for triple therapy?” and “Have my eosinophil levels been checked recently?” The answer could change everything.
What is triple inhaler therapy for COPD?
Triple inhaler therapy combines three medications - an inhaled corticosteroid (ICS), a long-acting muscarinic antagonist (LAMA), and a long-acting beta-agonist (LABA) - to reduce airway inflammation, open the lungs, and control mucus. It’s used for patients with moderate-to-severe COPD who have frequent exacerbations and high blood eosinophil counts (≥300 cells/µL).
Does triple therapy reduce COPD exacerbations?
Yes, for the right patients. Clinical trials show a 20-25% reduction in moderate-to-severe exacerbations when triple therapy is used in people with eosinophil counts ≥300 cells/µL. In real-world settings, the benefit is strongest when switching from multiple inhalers to a single-device system.
Is triple inhaler therapy better than dual therapy?
For patients with frequent exacerbations and high eosinophils, triple therapy offers a clear advantage over LAMA/LABA alone. But for those with low eosinophils (<100 cells/µL), there’s no benefit - and a higher risk of pneumonia. The decision must be based on biomarkers, not just disease severity.
What are the risks of triple inhaler therapy?
The biggest risk is pneumonia, especially with fluticasone-based inhalers. Studies show a 1.83-fold higher risk compared to budesonide-based options. Other risks include oral thrush, hoarseness, and potential bone density loss with long-term steroid use. Regular monitoring and proper inhaler technique help reduce these risks.
Why is single-inhaler therapy better than multiple inhalers?
Single-inhaler therapy improves adherence by 15-20% because patients are less likely to forget doses or get confused. Studies show patients switching from multiple inhalers to one device report fewer exacerbations and better quality of life. Simplicity leads to consistency - and consistency leads to better outcomes.
How do I know if I’m a candidate for triple therapy?
You’re a candidate if you’ve had two or more moderate exacerbations, or one severe exacerbation requiring hospitalization in the past year, AND your blood eosinophil count is 300 cells/µL or higher. Your doctor should test this before prescribing. If your count is below 100, triple therapy is not recommended.
Can I stop using my triple inhaler if I feel better?
No - not without talking to your doctor. COPD is a chronic condition. Feeling better doesn’t mean the underlying inflammation is gone. Stopping ICS suddenly can trigger a rebound in inflammation and worsen exacerbations. Always follow your provider’s guidance on adjustments.
Are there cheaper alternatives to brand-name triple inhalers?
Generic versions of triple inhalers are limited. Some patients use multiple-inhaler combinations (LAMA + LABA + ICS) to lower costs, but this reduces adherence. Insurance coverage varies - ask about patient assistance programs or mail-order options. Never skip doses due to cost; talk to your provider about alternatives.