Most people don’t think about their bones until they break. But by then, it’s often too late. Osteoporosis doesn’t come with warning signs - no pain, no swelling, no redness. It’s silent. That’s why DEXA scan results matter more than you might realize. If you’re over 65, or have risk factors like early menopause, long-term steroid use, or a family history of hip fractures, getting screened isn’t optional - it’s essential.
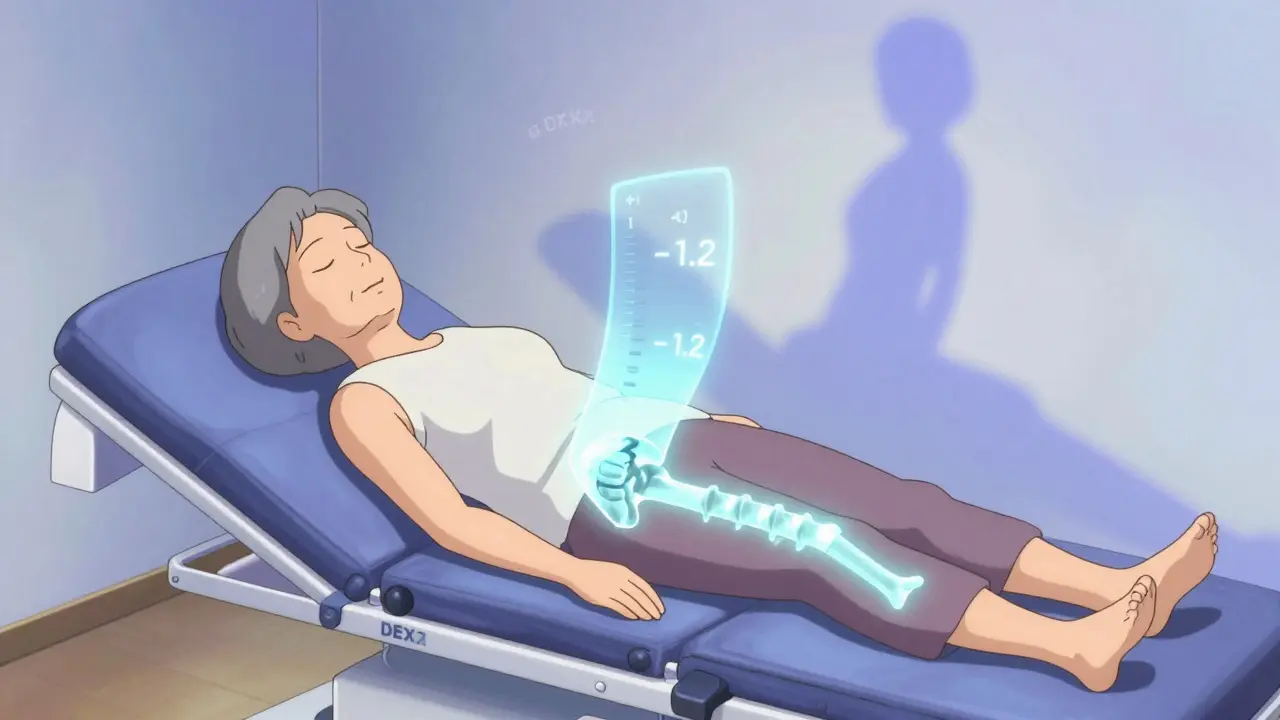
What a DEXA Scan Actually Measures
A DEXA scan isn’t just another X-ray. It’s a precise, low-dose imaging test that measures how much mineral - mostly calcium - is packed into your bones. The machine sends two different X-ray beams through your hip and spine. By comparing how much of each beam gets absorbed, it calculates your bone mineral density (BMD) in grams per square centimeter. The whole thing takes about 10 minutes. You lie still on a table, fully clothed. No needles. No fasting. No discomfort.
The radiation you get from a DEXA scan is less than what you’d absorb from a cross-country flight or two days of natural sunlight. That’s why it’s safe to repeat every two years if needed. It’s also why it’s the gold standard. No other test - not ultrasound, not peripheral scans, not even CT scans - has been proven as reliably linked to actual fracture risk across diverse populations.
Understanding Your T-Score: The Key to Your Bone Health
Your DEXA report will show a number called the T-score. This is the most important number on the page. It tells you how your bone density compares to that of a healthy 30-year-old adult of the same sex and ethnicity.
- T-score of -1.0 or higher: Normal bone density. Your bones are in good shape.
- T-score between -1.0 and -2.5: Osteopenia. Your bones are weaker than normal, but not yet osteoporotic. This is your wake-up call.
- T-score of -2.5 or lower: Osteoporosis. Your bones are significantly fragile. Fracture risk rises sharply here.
Let’s say your T-score is -2.7. That doesn’t mean you’ll definitely break a bone. But it does mean your risk is 4 to 5 times higher than someone with a normal T-score. The lower the number, the greater the risk. A T-score of -3.0 isn’t just “a bit worse” than -2.5 - it’s a major red flag.
Many people panic when they see “osteopenia.” But it’s not a diagnosis of disease - it’s a signal to act. Lifestyle changes can still reverse bone loss at this stage. Medication might be needed, but only if other risk factors are present.
Why Z-Score Alone Doesn’t Tell the Whole Story
Your report might also list a Z-score. This compares your bone density to people your own age. If you’re 72 and your Z-score is -1.5, that might sound alarming. But if most people your age have low bone density, then your score isn’t unusual - just expected.
Doctors use Z-scores mainly for younger adults or children. For postmenopausal women and men over 70, the T-score is what matters. A Z-score that’s normal doesn’t mean your bones are safe. You could still have osteoporosis if your bones are thinner than those of a healthy young adult.
Fracture Risk Isn’t Just About Bone Density
Here’s the truth: not everyone with a T-score of -2.8 will break a bone. And not everyone with a T-score of -1.8 will stay fracture-free. Bone density alone doesn’t tell the full story. That’s why doctors use the FRAX tool.
FRAX is a free online calculator developed by the World Health Organization. It takes your T-score and adds in your age, sex, weight, smoking status, alcohol intake, history of prior fractures, family history of hip fracture, and whether you’re on steroid medication. It then gives you a percentage - your 10-year risk of a major osteoporotic fracture (hip, spine, forearm, shoulder).
For example: a 70-year-old woman with a T-score of -2.3, who smokes, weighs 110 pounds, and had a previous wrist fracture, might have a 22% risk of fracture in the next decade. That’s high enough to start treatment - even if her T-score isn’t yet in the osteoporosis range.
On the flip side, a 68-year-old woman with a T-score of -2.6 but no other risk factors, who exercises daily, doesn’t smoke, and drinks little alcohol, might have only a 10% risk. She might be monitored instead of treated immediately.
FRAX turns a single number into a real-world picture. That’s why it’s now standard practice in the UK and US.

What DEXA Can’t Tell You
DEXA is excellent - but it has limits. It can’t tell you how strong your bone structure is internally. Two people with the same BMD can have very different fracture risks because of differences in bone microarchitecture.
That’s where new tools like Trabecular Bone Score (TBS) come in. TBS analyzes the texture of your spine on the DEXA image to estimate how spongy or brittle your internal bone structure is. Studies show adding TBS improves fracture prediction by up to 18%. Some clinics in the UK now offer it alongside standard scans.
DEXA also struggles in people with severe arthritis, spinal fusion, or aortic calcifications. Metal implants can distort results. If your scan looks odd, your doctor might recommend a different test - like a VFA (vertebral fracture assessment), which checks for hidden spinal fractures you didn’t even know you had.
Who Should Get Screened - And When
In the UK and US, guidelines are clear:
- All women 65 and older
- All men 70 and older
- Postmenopausal women under 65 with risk factors (low body weight, smoking, steroid use, family history)
- Men 50-69 with risk factors
- Anyone who’s broken a bone after age 50 from a minor fall
- People on long-term steroid therapy (more than 3 months)
Medicare and most UK private insurers cover DEXA scans every two years for eligible patients. But here’s the problem: only about 40% of women over 65 get screened. And the gap is wider among Black and Hispanic women - only about 20% get tested, despite similar or higher fracture risks.
If you’re unsure whether you qualify, ask your GP. Don’t wait for symptoms. By the time you feel pain from a spinal fracture, the damage is already done.
What Happens After Your Scan
If your results are normal: keep doing what you’re doing. Weight-bearing exercise, enough vitamin D, and protein intake are your best defenses.
If you have osteopenia: focus on lifestyle. Walk 30 minutes a day. Lift light weights twice a week. Get your vitamin D checked. Most people don’t need medication yet - but they do need a plan.
If you have osteoporosis: treatment is usually recommended. Options include bisphosphonates (like alendronate), denosumab injections, or newer drugs like romosozumab. These aren’t magic bullets - they reduce fracture risk by 30-70% over 3-5 years. But they only work if taken consistently.
And yes, you’ll need follow-up scans. Not every year. Usually every 2-3 years, unless you’re on strong medication. Too many scans don’t help - they just add cost and anxiety.

Real Stories, Real Impact
A 71-year-old woman in Bristol came in for a routine DEXA scan after her sister broke her hip. Her T-score was -2.8. No pain. No history of falls. She thought she was fine. The scan showed a hidden spinal fracture - one she’d never noticed. She started treatment. Within a year, her bone density improved. She’s now walking daily, lifting groceries, and not afraid to bend over.
That’s the power of screening. It doesn’t just detect disease. It prevents tragedy.
Common Misconceptions
- “I’m young, so I don’t need this.” Osteoporosis isn’t just an older person’s disease. Early menopause, eating disorders, or long-term steroid use can cause bone loss in your 40s.
- “I take calcium - that’s enough.” Calcium alone won’t fix bone loss. You need vitamin D, exercise, and sometimes medication.
- “DEXA is dangerous.” The radiation is less than a day’s natural exposure. You’re safer getting screened than ignoring it.
- “My doctor said I’m fine.” If your doctor didn’t mention your T-score or FRAX risk, ask for it. Don’t assume they’re on top of it.
What to Do Next
If you’re in your 50s or older:
- Check your risk factors: age, gender, weight, smoking, steroid use, prior fractures.
- Ask your GP: “Do I need a DEXA scan?”
- If you’ve had a fracture after 50, get one now - don’t wait.
- If your T-score is below -1.0, ask about FRAX.
- Start walking. Start lifting. Start protecting your bones - before they break.
Bone health isn’t about supplements. It’s about awareness. It’s about knowing your numbers. And it’s about acting before it’s too late.
What is a normal DEXA scan result?
A normal DEXA result means your T-score is -1.0 or higher. This indicates bone density within the range of a healthy young adult. You don’t have osteopenia or osteoporosis, but maintaining bone health through exercise, vitamin D, and protein intake is still important.
Can I get a DEXA scan without a doctor’s referral?
In the UK, most NHS and private clinics require a referral from your GP or specialist. Some private clinics offer self-referral, but insurance usually won’t cover it unless there’s a medical indication. Always check with your provider first.
Is a DEXA scan painful?
No, it’s completely painless. You lie on a table while the machine passes over your body. It’s similar to an X-ray, but quieter and faster. Most people describe it as comfortable, even relaxing.
How often should I get a DEXA scan?
For most people, every two years is standard. If your results are normal and you have no risk factors, you might wait longer. If you’re on treatment for osteoporosis, your doctor may repeat the scan after 1-2 years to check progress. More frequent scans aren’t helpful and can increase anxiety without improving outcomes.
Can men get osteoporosis?
Yes. While more common in women, 1 in 5 men over 50 will have an osteoporosis-related fracture. Risk increases with age, low testosterone, steroid use, smoking, and alcohol. Men over 70 should be screened - and those with risk factors should start at 50.
Does insurance cover DEXA scans?
In the UK, NHS covers DEXA scans for people who meet clinical criteria. Private insurance typically covers it too if referred by a GP. Medicare in the US covers scans every two years for eligible patients. Always confirm coverage with your provider before scheduling.