Eosinophilic esophagitis isn't just heartburn that won’t go away. It’s a chronic immune reaction in the esophagus, triggered by everyday foods, that turns swallowing into a painful, sometimes terrifying experience. Imagine choking on a bite of bread or struggling to get a sip of water down-no matter how hard you try. That’s the reality for more than 160,000 people in the U.S. alone, with numbers rising fast. Unlike acid reflux, EoE doesn’t respond to antacids. It needs a targeted approach: either removing the foods that set off the immune response or using special steroid treatments that coat the esophagus directly.
What Exactly Is Eosinophilic Esophagitis?
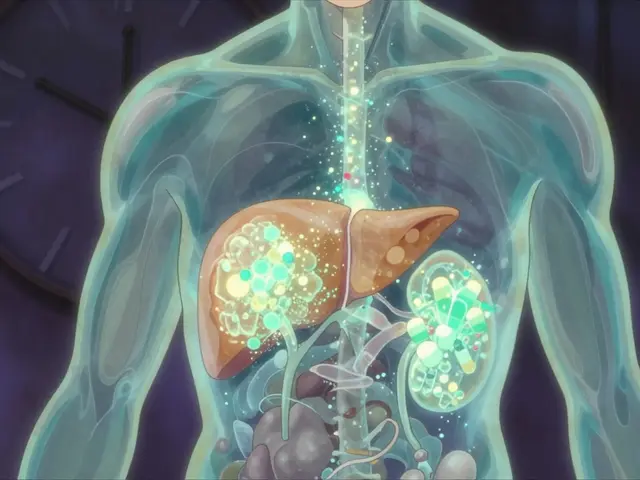
Eosinophilic esophagitis, or EoE, happens when too many eosinophils-white blood cells that usually fight parasites-pile up in the lining of your esophagus. These cells don’t belong there. When they show up in large numbers, they cause inflammation, scarring, and narrowing. Over time, the esophagus can lose its ability to stretch and move food down properly. That’s why many patients end up needing a procedure called dilation, where a doctor gently widens the narrowed area.
This condition was only recognized as its own disease in the early 2000s. Before that, it was often mistaken for GERD. The key difference? GERD responds to acid blockers. EoE doesn’t. It’s driven by allergies-not stomach acid. The immune system sees certain foods as invaders and sends eosinophils to attack. That’s why diet plays such a central role in treatment.
The Big Six: Most Common Food Triggers
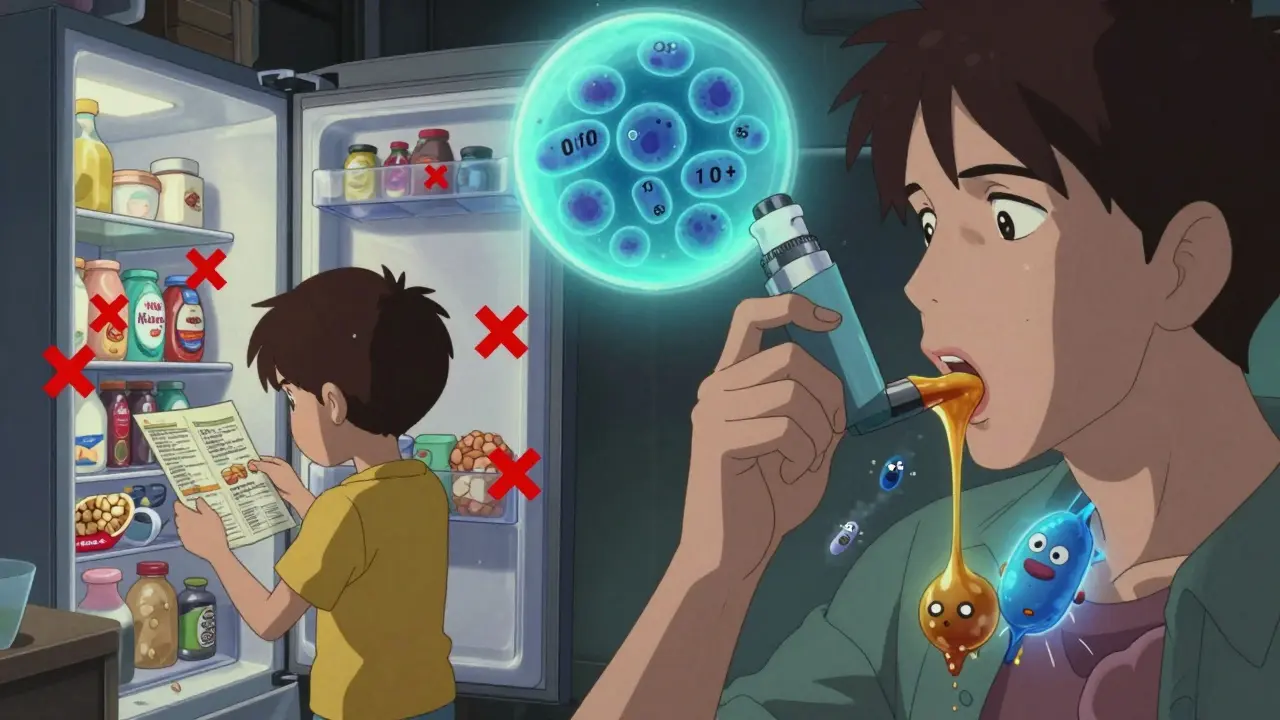
Not all foods trigger EoE equally. Research shows a small group of foods is responsible in the vast majority of cases. The six-food elimination diet targets the most common culprits: milk, eggs, wheat, soy, fish/shellfish, and nuts. These foods account for over 90% of identified triggers in clinical studies.
But here’s the surprising part: you don’t always need to cut out all six. A landmark 2022 NIH study found that removing just milk-the single most common trigger-led to remission in 64% of adult patients. That’s nearly as effective as removing all six foods. For kids, the six-food diet still works better, with remission rates hitting 75-80%. But for adults, starting with milk alone can be a game-changer. It’s less restrictive, easier to stick with, and still highly effective.
Some people find other triggers. Soy is more common in Europe than in the U.S. Legumes, like lentils or chickpeas, can also cause reactions. But for most, it’s the big six. The key is not guessing. You don’t rely on skin prick tests or blood tests-they’re only 20-30% accurate for EoE. The only reliable way to find your triggers is through elimination and careful reintroduction, backed by an endoscopy to confirm healing.
Steroid Slurries: How They Work and How to Use Them
If diet feels too overwhelming-or if you need faster relief-steroid slurries are the next step. These aren’t inhaled asthma medications. They’re topical steroids, like fluticasone or budesonide, mixed into a thick liquid so you swallow them instead of breathing them in.
Here’s how it works: you take a standard inhaler dose-say, 220 mcg of fluticasone-and mix it with 2-3 mL of water, honey, or applesauce. You swish it around your mouth for 30 seconds, then swallow. The goal is to coat the esophagus, not let the steroid get absorbed into your lungs. This direct delivery reduces inflammation where it matters most.
Budesonide oral suspension, sold as Jorveza, was approved by the FDA in January 2023 specifically for EoE. It’s formulated to stay in the esophagus longer. In clinical trials, 64% of patients achieved histological remission (meaning fewer than 15 eosinophils per high-power field under the microscope) after 12 weeks. That’s compared to just 2% in the placebo group.
Fluticasone is cheaper and more widely available, but it’s not approved for EoE-it’s used off-label. Studies show it works in 50-60% of cases. Budesonide works faster and slightly better, but it’s more expensive. Both take 4-8 weeks to show real improvement. Many patients feel better in 2 weeks, but the tissue healing takes longer.
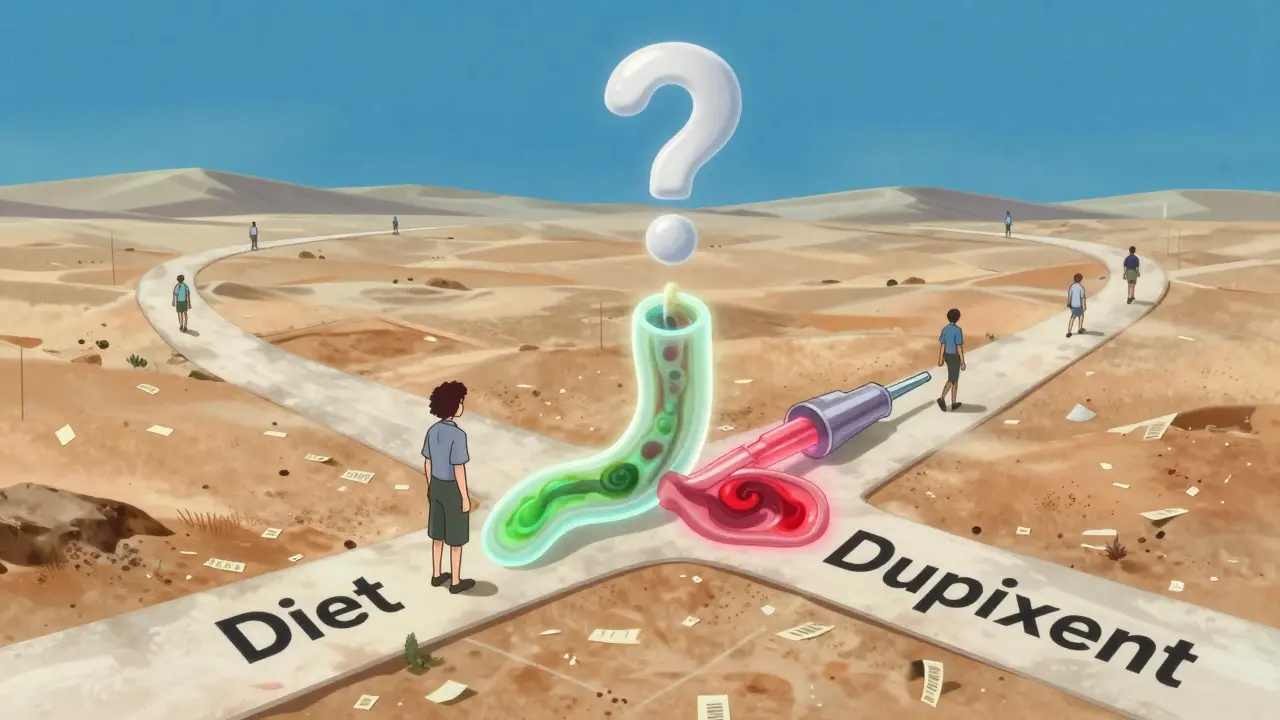
Pros and Cons: Diet vs. Steroids
Choosing between diet and steroids isn’t about which is better-it’s about what fits your life.
Dietary elimination has no side effects. No oral thrush. No risk of systemic steroid exposure. It can lead to long-term remission if you avoid your triggers. But it’s hard. It means reading every label, avoiding restaurants, and explaining your diet to everyone you eat with. About 62% of patients say they struggle to keep it up long-term. And if you’re not careful, you can become deficient in calcium, vitamin D, or protein-especially if you cut out dairy.
Steroid slurries work faster. Most people feel less pain and better swallowing within 2-4 weeks. But they come with trade-offs. Around 15% of users get oral thrush-a fungal infection that causes white patches and discomfort in the mouth. Rinsing with water after swallowing helps, but doesn’t always prevent it. Some patients hate the taste. Honey helps mask it, but not everyone likes the idea of swallowing sweetened steroids. And if you stop the medication, symptoms often come back.
There’s no one-size-fits-all. Many people start with diet. If that doesn’t work fast enough, they add steroids. Others use steroids first to get quick relief, then transition to diet to reduce long-term reliance on medication. Some use both together.
What Happens After Treatment?
Remission doesn’t mean you’re cured. It means the inflammation is under control. But EoE is chronic. The immune system doesn’t forget its triggers.
After 8-12 weeks of treatment, your doctor will likely schedule another endoscopy. That’s the only way to confirm healing. Symptoms can improve before the tissue does. You might feel fine, but if eosinophils are still high, the damage keeps building.
Reintroducing foods is a slow, careful process. You add one food back every 2-3 weeks. If your symptoms return, you know that’s your trigger. If not, you keep going. It’s tedious, but it’s the only way to find out what you can safely eat again.
Even after finding your triggers, many patients need to stay on a modified diet for life. Some can tolerate small amounts. Others can’t. And if you stop avoiding your triggers, inflammation returns-often within months.
Support and Resources
You don’t have to do this alone. The American Partnership for Eosinophilic Disorders (APFED) offers free dietitian consultations and meal planning tools. The Cincinnati Center for Eosinophilic Disorders runs a food pantry that provides free hypoallergenic meals to qualifying patients. Online communities like Reddit’s r/EoE have over 8,000 members sharing tips, recipes, and emotional support.
For those struggling with cost, Jorveza and Dupixent (a newer biologic approved in May 2023) may be covered by insurance, especially if you’ve tried diet and steroids first. Dupixent, originally for eczema and asthma, reduces inflammation by blocking key immune signals. In trials, it helped 60% of patients achieve remission after 24 weeks. It’s a shot given every two weeks-not a daily pill-but it’s changing the game for adults who can’t tolerate dietary restrictions.
What’s Next for EoE Treatment?
The future is moving toward precision. Researchers are working on blood tests that can predict food triggers without elimination diets. One study is looking at specific proteins in milk-like casein-rather than cutting out all dairy. If they can identify exactly which protein triggers your reaction, you might be able to avoid just that one component.
Biologics like Dupixent are the biggest breakthrough in decades. They target the immune system’s overreaction directly. They’re not a cure, but they’re giving people back their lives without the constant fear of choking.
For now, the two pillars remain: diet and steroid slurries. Both work. Both have downsides. But together, they give you control. You can choose what fits your body, your schedule, and your tolerance for risk.
There’s no magic bullet. But there is hope. And with the right plan, most people with EoE can eat, swallow, and live without fear.
Can you outgrow eosinophilic esophagitis?
Most people don’t outgrow EoE. It’s a lifelong condition. Symptoms can improve with treatment, and some children may see fewer issues as they age, but the immune system usually stays sensitive to triggers. Stopping dietary restrictions or medication often leads to a return of symptoms. Long-term management is the norm, not the exception.
Do allergy tests help find EoE triggers?
Skin prick tests and blood tests for IgE antibodies are not reliable for EoE. They only identify about 20-30% of true food triggers. That’s because EoE is often driven by non-IgE-mediated reactions. The only proven way to find triggers is through elimination diets followed by systematic reintroduction, confirmed by endoscopy.
Is budesonide better than fluticasone for EoE?
Budesonide oral suspension (Jorveza) is specifically designed for EoE and has stronger clinical data. In trials, it achieved 64% remission compared to 50-60% for fluticasone. It also acts faster and has better tissue retention. However, fluticasone is cheaper and more accessible. Both require proper technique-swishing and swallowing, not inhaling. If cost or availability is an issue, fluticasone can still be effective.
Can you use steroid slurries long-term?
Steroid slurries are usually used for 8-12 weeks to induce remission. Long-term daily use isn’t recommended because of the risk of oral thrush and potential systemic absorption. Some patients use them intermittently during flare-ups, under a doctor’s supervision. The goal is to use them as a bridge to dietary control or newer biologics like Dupixent, which can provide longer-term control without daily steroids.
What should you do if steroid slurries don’t work?
If steroids don’t improve symptoms after 12 weeks, your doctor may recommend switching to a different approach-like a stricter elimination diet, or moving to a biologic medication like Dupixent. Dupilumab, approved in 2023, works by blocking key inflammatory signals and has shown success in patients who didn’t respond to diet or steroids. Endoscopic evaluation is critical to determine if inflammation persists and guide next steps.