What You’re Seeing on Your Prescription Bottle
Open your last prescription bottle. Look at the label. You’ll see a big, bold name-maybe Lipitor or Prozac. Below it, smaller and less obvious, is another name: atorvastatin or sertraline. That’s not a mistake. That’s how prescription labels work in the U.S. and the UK. The big name is the brand name. The small one is the generic name. They’re the same medicine. Just dressed differently.
Why Two Names? It’s Not a Trick
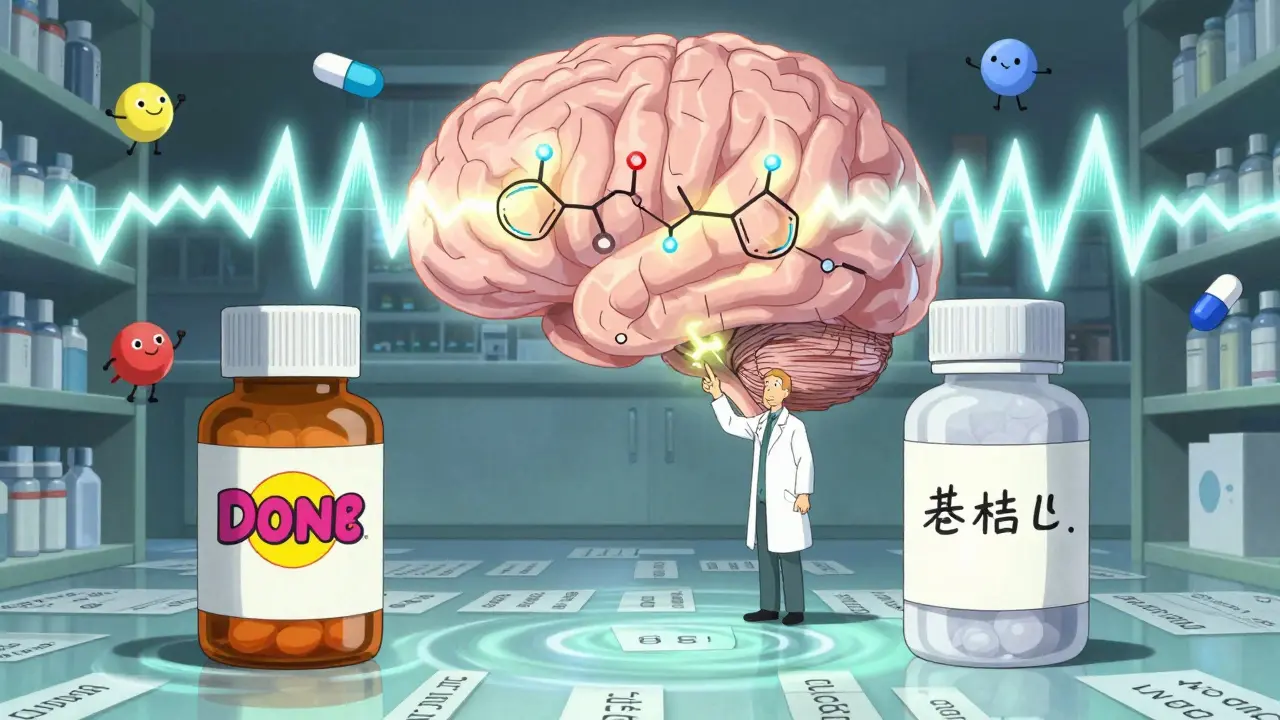
Pharmaceutical companies spend millions developing a new drug. They get a patent, which gives them exclusive rights to sell it under a unique brand name-like Prilosec for heartburn. Once the patent expires, other companies can make the same drug. But they can’t use the same brand name. So they call it by its chemical name: omeprazole. That’s the generic name.
The active ingredient? Identical. The dose? The same. How it works in your body? Exactly the same. The FDA requires generic drugs to meet the same strict standards as brand-name ones. They must deliver the same amount of medicine into your bloodstream within the same timeframe. That’s called bioequivalence. The numbers? The 90% confidence interval for absorption has to fall between 80% and 125% of the brand-name drug. That’s not a wide gap-it’s a tight, clinically safe range.
Cost Difference? It’s Huge
Here’s the real difference: price. A 30-day supply of brand-name Lipitor might cost $300. The generic atorvastatin? Around $4. That’s not a typo. Generic drugs save patients and the system billions every year. From 2007 to 2016, generics saved the U.S. healthcare system $1.67 trillion. In 2022, 90% of all prescriptions filled in the U.S. were for generics. Yet, they made up only 22% of total drug spending. Why? Because brand-name drugs are expensive. Their price covers the cost of research, clinical trials (which average $2.6 billion per drug), and marketing. Generics skip all that. They just prove they work the same way.
And here’s something most people don’t know: about half of all generic drugs are actually made by the same companies that make the brand-name versions. They just sell them under a different label. So when you pick up a generic, you might be getting the exact same pill, just without the fancy packaging.
Why Do They Look Different?
Ever opened a new bottle and thought, “Wait, this pill doesn’t look right”? That’s because of trademark law. Brand-name companies own the look of their pills-the color, the shape, the imprint. Generic manufacturers can’t copy that. So they make theirs different. A blue oval might become a white circle. A red capsule might turn into a yellow tablet. It’s not a change in effectiveness. It’s just a legal requirement.
But this causes confusion. One in seven medication errors involves someone mixing up pills because they look different. That’s why pharmacists are required to explain the switch. In 41 states, they must list both the brand and generic name on the label. And if you’re unsure? Ask. Most pharmacies will show you the label and point out both names.
What About Side Effects? Are Generics Less Safe?
Some people say, “I switched to the generic and felt different.” Maybe you had more stomach upset. Or you felt more tired. It’s understandable to wonder if the generic isn’t as good. But here’s the truth: the active ingredient is the same. So the core effect on your body shouldn’t change.
What can differ? The inactive ingredients. That’s the stuff that holds the pill together-fillers, dyes, coatings. Sometimes, one person’s body reacts to a dye or a coating in a generic version. It’s rare, but it happens. If you notice a change after switching, talk to your pharmacist. They can check if it’s an inactive ingredient issue. In most cases, switching back to the brand or trying a different generic fixes it.
There’s one exception: drugs with a narrow therapeutic index (NTI). These are medications where even tiny changes in blood levels can cause big problems. Think warfarin (blood thinner), lithium (for bipolar disorder), or some seizure meds. Some doctors prefer to stick with the brand-name version here, even though the FDA says generics are safe. It’s a cautious choice-not because generics are worse, but because the margin for error is razor-thin.
How Pharmacists Decide What to Give You
When your doctor writes a prescription, they usually just write the drug name. They don’t specify brand or generic. That’s intentional. Pharmacists are trained to substitute generics unless the doctor says “dispense as written” or “do not substitute.” In 28 states, substitution is automatic unless blocked. Most insurance plans require it too. Why? Because it saves money-for you and the system.
But you have rights. You can ask for the brand-name version. You can refuse the generic. You can even ask your pharmacist to show you both options side by side. If your insurance won’t cover the brand-name drug, you might pay more out of pocket. But you’re still in control.
What the Label Actually Tells You
Here’s how to read your Rx label like a pro:
- Top line: Usually the brand name (e.g., Prozac).
- Below it, smaller: The generic name (e.g., fluoxetine).
- Next: Strength (e.g., 20 mg).
- Then: Quantity and instructions (e.g., “Take one daily”).
- Bottom: Pharmacy name, date, and prescriber.
Ninety-two percent of prescription labels follow this format. If you don’t see both names, ask. You’re entitled to know what you’re taking.

Why This Matters for You
Understanding this isn’t just about saving money. It’s about avoiding confusion. You might get a refill and think it’s a different drug because the pill looks different. Or you might refuse a generic because you’re afraid it won’t work. That’s unnecessary fear. Generics are not second-rate. They’re the same medicine, just cheaper.
Studies show 78% of patients are satisfied with generics once they understand they’re equivalent. But 32% start out worried. Education cuts that fear by two-thirds. A quick chat with your pharmacist can prevent anxiety, missed doses, or even dangerous mistakes.
What’s Changing in 2026?
The FDA is speeding up generic approvals with its GDUFA III program, aiming for 20% faster reviews by 2027. More biologics-complex drugs like insulin or rheumatoid arthritis treatments-are losing patents. That means more “generic” versions called biosimilars will hit the market. They’re not exact copies like small-molecule generics, but they’re still 15-30% cheaper than the brand.
Medicare Part D is changing too. Starting in 2025, seniors won’t pay more than $2,000 a year for all their prescriptions. That will make generics even more attractive.
But there’s a risk. About 80% of the active ingredients in pills are made in China and India. Supply chain issues during the pandemic showed how fragile that system is. If a factory shuts down, you might get a different generic-or none at all. That’s why pharmacists sometimes switch brands mid-refill. It’s not a change in quality. It’s a change in availability.
Bottom Line: Same Drug. Different Price Tag.
Generic and brand-name drugs are not different in how they work. They’re the same medicine, made to the same standards. The only real difference is the price-and sometimes, the color of the pill.
If you’re unsure about your prescription, ask your pharmacist. They’re the experts on your meds. Don’t assume a different-looking pill is weaker. Don’t pay more just because it has a familiar name. And if you feel different after switching? Talk to someone. It’s not always the drug. Sometimes, it’s the dye.