Every year, over 107,000 people in the U.S. die from drug overdoses. Many of these deaths aren’t caused by one drug alone - they happen because of drug interactions that quietly multiply the danger. Mixing opioids with alcohol, benzodiazepines, or even some over-the-counter sleep aids can turn a routine dose into a life-threatening event. The good news? Most of these deaths are preventable. You don’t need to be a doctor to check for dangerous combinations. With the right questions and tools, you can spot the risks before it’s too late.
Why Some Drug Mixes Are Deadly
Not all drug interactions are the same. Some cause mild nausea or drowsiness. Others shut down your breathing. The deadliest combinations involve substances that all slow down your central nervous system (CNS). These include opioids like oxycodone or heroin, benzodiazepines like Xanax or Valium, alcohol, sleep medications like Ambien, and even some muscle relaxants. When these drugs are taken together, they don’t just add up - they multiply. A 2022 study in JAMA Internal Medicine found that mixing opioids and benzodiazepines increases the risk of fatal overdose by more than 10 times compared to opioids alone. Alcohol makes it worse. Research from the NIH shows that combining opioids with alcohol raises the chance of respiratory depression by 67%.This isn’t just about prescription drugs. Street drugs are often contaminated. What someone thinks is heroin might be fentanyl-laced cocaine. Fentanyl is 50 to 100 times stronger than morphine. Even a tiny amount can stop breathing - especially when mixed with another depressant. The CDC says 75% of opioid-related overdoses involve more than one substance. Most people don’t realize they’re at risk until it’s too late.
How Clinicians Check for Dangerous Interactions
Doctors and pharmacists use proven tools to catch these risks before they become emergencies. The CDC’s Opioid Risk Tool (ORT) is a five-question screening used in clinics across the U.S. It takes less than two minutes and identifies patients at high risk of misuse with 95% accuracy. But it’s not just about the tool - it’s about how the questions are asked. Asking, “Are you taking other medications?” often gets a simple “no.” Asking, “Do you ever take medicines not prescribed to you?” increases honest answers by 52%, according to a 2022 study in Addiction.Pharmacists use the Beers Criteria, updated every two years by the American Geriatrics Society, to flag risky combinations in older adults. For example, mixing opioids with antihistamines found in cold medicines can cause dangerous drowsiness in seniors. The FDA’s Drug Interaction Checker, updated monthly, helps professionals cross-reference over 1,200 medications. But these tools have a blind spot: they only cover legal, prescribed drugs. They don’t know about street drugs, shared pills, or substances bought online.
What Digital Tools Can - and Can’t - Do
There are dozens of apps and websites that claim to check drug interactions. Medscape’s Drug Interaction Checker, updated weekly, identifies 89% of known dangerous combinations between prescription drugs. The National Library of Medicine’s MedlinePlus database covers over 10,000 medications. These are great if you know exactly what you’re taking and it’s on a prescription label.But here’s the problem: 63% of dangerous interactions happen with substances that aren’t in these databases. That includes illicit drugs like fentanyl, methamphetamine, or counterfeit pills. A 2023 study by NIDA found that digital tools miss 78% of interactions involving fentanyl analogs because they’re not listed as approved medications. Even worse, many people don’t know what they’re actually taking. Street names like “Molly,” “Perks,” or “Blue” can mean anything - from MDMA to fentanyl. No app can warn you about that unless you tell it exactly what’s in the pill.
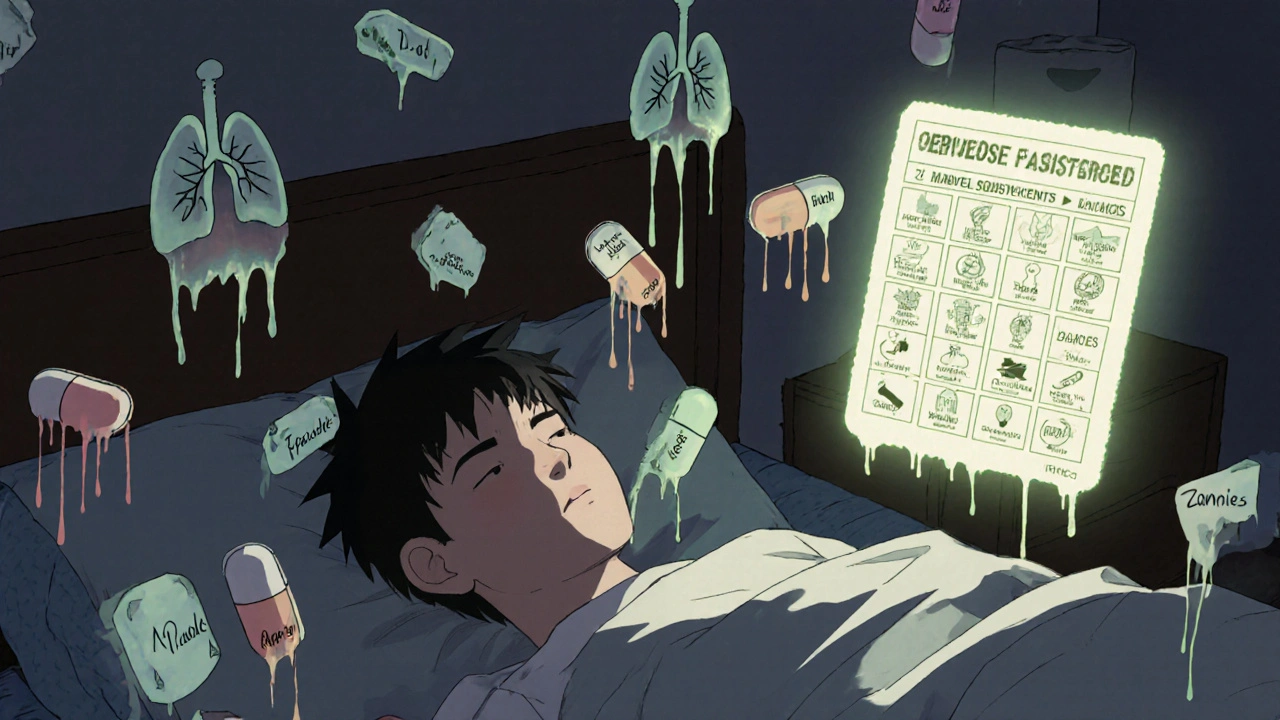
How to Check for Interactions If You’re Not in a Clinic
If you’re not seeing a doctor regularly, you still have options. The National Harm Reduction Coalition offers a free, downloadable “Overdose Risk Self-Check” tool. It’s a 10-question quiz based on clinical guidelines, available in 12 languages. It doesn’t ask for medication names - it asks about effects and street terms. Questions like: “Have you used any pills or powders that weren’t prescribed to you in the last week?” or “Do you ever take something to help you sleep or calm down with your pain meds?”Another effective method is using the “Overdose Risk Assessment Card” - a physical card used by outreach workers in communities. It lists 23 common substances with their street names: Xanax (bars, zannies), alcohol (booze, juice), cocaine (coke, crack), fentanyl (apache, dance fever), etc. You simply point to what you’ve used. This reduces shame and increases honesty. In focus groups, people who refused to admit to taking Valium told the truth when asked if they’d used “downers.”
What You Need to Know About Street Drugs
One of the biggest gaps in overdose prevention is the assumption that people know what’s in the drugs they’re using. They don’t. In 2023, the DEA reported that over 60% of fake pills tested contained a lethal dose of fentanyl. Many users think they’re taking oxycodone or Adderall, but they’re actually taking something far more dangerous. Mixing fentanyl with alcohol or benzodiazepines is like lighting a fuse on a bomb.Learn the common street names for depressants:
- Benzodiazepines: Xanax = bars, zannies, benzos; Valium = vallies, blues
- Alcohol: juice, liquor, hooch
- Sleep aids: zzz’s, z-drugs, Ambien = sleeping pills
- Fentanyl: apache, dance fever, china white, TNT
- MDMA: Molly, ecstasy, beans
If you’re using any of these, assume the worst: they might be cut with fentanyl. Even if you’ve used them before without issue, today’s batch could be deadly. There’s no safe way to use illicit drugs - but knowing the risks can help you make smarter choices.
Who’s at Highest Risk?
Some people are more vulnerable to overdose from drug interactions:- People who’ve stopped using for a while: Tolerance drops fast. After just 72 hours without opioids, your body loses 30-50% of its tolerance. Going back to your old dose can kill you.
- People with breathing problems: Asthma, COPD, or sleep apnea make respiratory depression more likely. Risk goes up 4.2 times.
- People who inject drugs: Injecting increases overdose risk by 300% compared to swallowing pills. Faster delivery = faster shutdown of breathing.
- Older adults: The Beers Criteria lists 56 risky combinations for seniors, including mixing opioids with antihistamines or muscle relaxants.
- People taking multiple prescriptions: The more meds you take, the higher the chance of a hidden interaction.
If any of these apply to you or someone you care about, extra caution is needed.

What to Do If You Suspect a Dangerous Mix
If you think you or someone else might be mixing dangerous drugs, here’s what to do:- Don’t wait for symptoms. Drowsiness, slow breathing, or confusion are warning signs - but they can come on fast.
- Carry naloxone. Naloxone (Narcan) reverses opioid overdoses. It doesn’t work on benzodiazepines or alcohol, but it can save a life if opioids are involved. It’s free and available without a prescription in most U.S. states.
- Use a drug checking kit. These small test strips (available through harm reduction groups) can detect fentanyl in powders or pills. Even if you don’t know what’s in it, you can find out if it’s lethal.
- Talk to someone. Whether it’s a pharmacist, a peer, or a hotline, telling someone reduces isolation and increases safety. A 2023 SAMHSA survey found that 68% of people who used drugs were never asked about alcohol or benzodiazepine use - even when prescribed opioids.
- Never use alone. If you use drugs, have someone nearby who knows what you took and how to respond. Most overdose deaths happen when people are alone.
What’s Changing in 2025
The landscape is shifting. As of January 2024, 38 U.S. states now require doctors to check for drug interactions before prescribing opioids. The FDA’s Drug Interaction Checker was updated in February 2024 to include 47 new fentanyl analogs. SAMHSA now requires all federally funded overdose prevention programs to screen for illicit substances - not just prescriptions.AI tools are also emerging. A 2023 study showed machine learning models could predict dangerous polydrug use from electronic health records with 92% accuracy. But privacy concerns remain. The most effective approach still combines technology with human connection. As Dr. Sarah Wakeman said in NEJM Catalyst: “The most effective risk assessment combines digital tools with empathetic questioning.”
The bottom line? Overdose deaths from drug interactions aren’t accidents. They’re failures of awareness - and awareness can be taught. You don’t need a medical degree to ask the right questions. You just need to care enough to look.
Can over-the-counter meds cause dangerous interactions with opioids?
Yes. Common OTC drugs like diphenhydramine (Benadryl), doxylamine (Unisom), and even some cough syrups with dextromethorphan can slow breathing when mixed with opioids. These are CNS depressants too. Many people don’t realize they’re taking them because they’re sold without a prescription. Always check labels for sedating ingredients if you’re on opioids.
How long does it take for tolerance to drop after stopping opioids?
Tolerance drops significantly within 72 hours. Studies show a 30-50% loss in tolerance after just three days without using. This is why people who’ve been in rehab, jail, or detox are at high risk of overdose if they return to their previous dose. Never assume your old tolerance still applies.
Is naloxone effective if someone mixed alcohol and opioids?
Naloxone only reverses opioid effects - not alcohol or benzodiazepines. But if opioids are part of the mix, naloxone can still save a life. It’s always worth administering. Call emergency services immediately, even if naloxone works. The other drugs may still cause breathing problems after the opioid is reversed.
Can drug interaction apps detect fentanyl in pills?
No. Apps and online checkers only work with known medications listed in their databases. Fentanyl analogs and counterfeit pills aren’t in these systems. The only way to detect fentanyl is with test strips - available for free from harm reduction organizations. Never rely on an app to tell you if a pill is safe.
Why do people lie about their drug use to doctors?
Fear of judgment, shame, or being denied treatment. Many patients worry they’ll be labeled as “addicts” or lose access to pain meds. Studies show that when providers ask non-judgmental questions like “Do you ever take medicines not prescribed to you?” instead of “Are you taking other drugs?”, disclosure rates jump by over 50%. Honest answers save lives.
What’s the safest way to reduce risk if I use multiple substances?
The safest way is to avoid mixing CNS depressants altogether. If you do use multiple substances, never use alone, carry naloxone, use a test strip if available, and start with a smaller dose than usual. Talk to a harm reduction worker - they’ve seen it all and won’t judge. Your life is worth more than secrecy.