When the temperature rises, most people think about staying cool, drinking water, and avoiding the sun. But for seniors taking certain medications, heat isn’t just uncomfortable-it can be deadly. Every year, more than 600 Americans die from heat-related causes, and nearly half of them are over 65. The real danger? Many of these deaths aren’t just from the heat itself. They’re from the way common medications interfere with the body’s ability to handle it.
Which Medications Make Heat More Dangerous?
Not all meds are created equal when it comes to heat. Some directly mess with how your body cools down. Diuretics like hydrochlorothiazide and furosemide are among the biggest culprits. These drugs help with high blood pressure and swelling, but they also make you pee more-and lose thirst. A 2022 study found seniors on diuretics feel 30-40% less thirsty, even when they’re dehydrated. That means they don’t drink enough, and their blood volume drops by 10-15%, making them prone to dizziness, falls, and fainting. ACE inhibitors and ARBs-meds like benazepril and losartan-also reduce thirst by about 25%. On their own, they’re safe. But when combined with diuretics, the risk spikes. Electrolytes like sodium can crash below 135 mmol/L, which triggers confusion, muscle weakness, and even seizures. Antipsychotics like quetiapine and clozapine, often given to seniors with dementia, block the brain’s thermostat. Research from the Mayo Clinic shows these drugs can raise core body temperature by 1.5-2.0°F without the person even feeling hot. That’s dangerous because heat stroke can sneak up without warning. Then there are anticholinergics-meds like diphenhydramine (Benadryl) and Tylenol PM. These stop sweating. And sweating is how your body cools itself. Clinical trials show these drugs can cut sweat production by 35-50%. If you can’t sweat, your body temperature climbs fast. Add sun exposure, and the risk of sunburn jumps 400-600% if you’re on certain antibiotics or antifungals.Why Seniors Are More at Risk
It’s not just the meds. Aging changes how your body works. Older adults have less water in their bodies, weaker sweat glands, and slower blood flow. Their kidneys don’t hold onto fluids as well. And many have heart disease, diabetes, or kidney problems-all of which make heat harder to handle. Add to that: 87% of seniors over 65 take two or more prescription drugs. That means the risk isn’t from one med-it’s from combinations. A diuretic plus an ACE inhibitor plus an anticholinergic? That’s a triple threat. The CDC says these combos are behind 22% of heat-related falls in older adults.What to Do Before Summer Hits
Don’t wait for a heat wave to act. Before temperatures start climbing, schedule a medication review with your doctor or pharmacist. Ask these questions:- Which of my meds make me more sensitive to heat?
- Should I adjust my dose on hot days?
- Do I need to change my fluid restrictions?
- Are there safer alternatives for any of these drugs?
Hydration: It’s Not Just About Drinking Water
Drink water. Yes. But it’s not that simple. If you’re on a diuretic, plain water isn’t enough. You need electrolytes. The American Geriatrics Society recommends drinking 8-10 eight-ounce glasses of water daily in hot weather. But if you’re on a fluid restriction due to heart failure, don’t just drink more-talk to your doctor. About 43% of heart failure patients on fluid limits develop dangerous electrolyte imbalances during heat waves. Choose drinks with 120-150 mg of sodium per 8 ounces. Sports drinks, oral rehydration solutions, or even broth can help. Avoid caffeine and alcohol. Both make you pee more and dry you out faster. One beer or cup of coffee can increase urine output by 40-60%.Stay Cool, Even If You Don’t Feel Hot
Air conditioning isn’t a luxury-it’s medical equipment for many seniors. Keep indoor temps below 78°F (25.6°C). If you don’t have AC, go to a library, mall, or community center. Arizona’s Haven Health reported a 29% drop in heat incidents after encouraging residents to spend midday hours in cooled spaces. Wear loose, light-colored cotton clothes. They let air flow and reflect sunlight. Synthetic fabrics trap heat and can raise your perceived temperature by 5-7°F. Use broad-spectrum sunscreen with SPF 15 or higher. Reapply every two hours-or after sweating. Some meds make your skin burn faster. The FDA says certain antibiotics and antifungals can increase sunburn risk by up to six times.What Caregivers Should Watch For
Seniors don’t always show the classic signs of heat stress. They might not sweat. They might not complain of thirst. Instead, look for subtle changes: confusion, slurred speech, irritability, or being unusually quiet. A 2023 UCLA study found that 78% of seniors showed early cognitive changes before physical symptoms appeared. Check in daily. Use the "I’m OK" program model: ask them if they’re feeling okay, check their temperature with a thermometer, and note any changes in behavior. Parkwood Heights senior living saw a 33% drop in hospitalizations after implementing daily check-ins.
Warning Signs You Can’t Ignore
Heat exhaustion looks like: heavy sweating, muscle cramps, headache, nausea, dizziness, fatigue, or fainting. If you see these, act fast. Move to a cool place. Drink cool water. Sponge off with cool water. Lie down. Heat stroke is an emergency. Signs include: body temperature above 103°F, hot dry or damp skin, rapid pulse, confusion, or loss of consciousness. This is life-threatening. Call 911 immediately. Don’t wait. The CDC says 65% of heat exhaustion cases turn into heat stroke within 2-4 hours if untreated.New Tools to Help
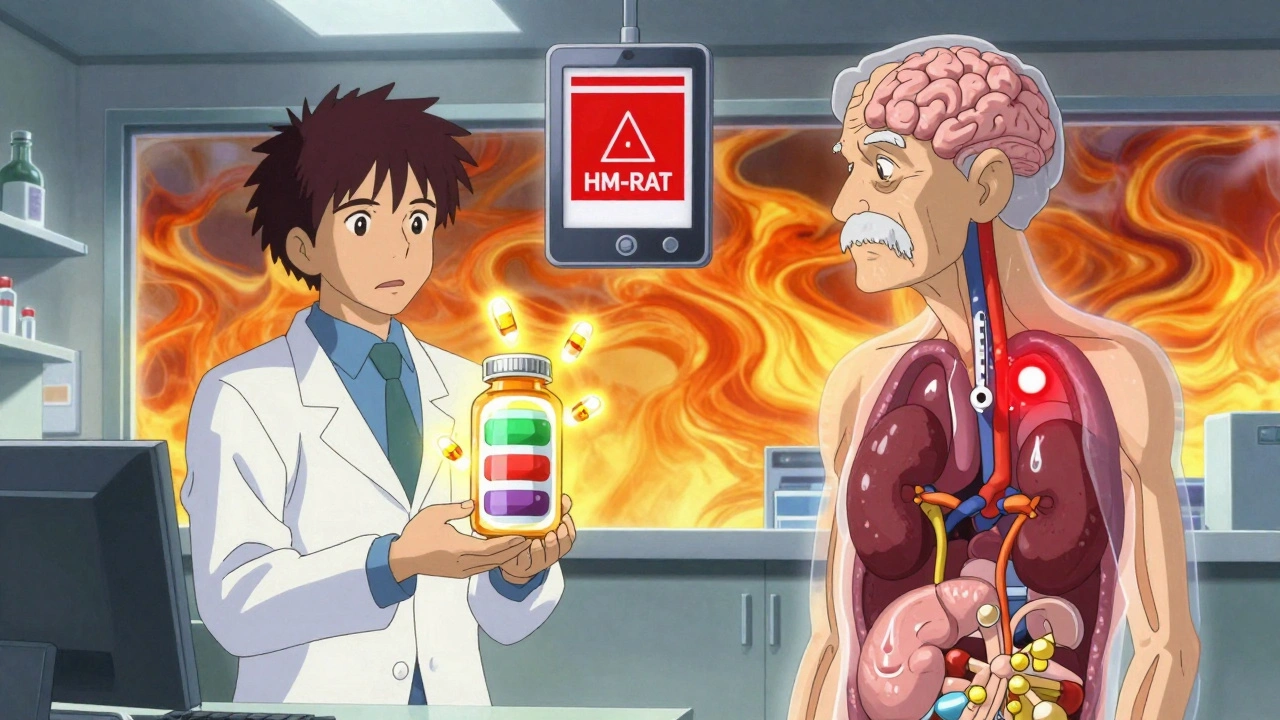
The CDC launched the Heat and Medication Risk Assessment Tool (HM-RAT) in June 2023. It lets you enter your meds and your zip code to get a personalized heat risk score. The National Institute on Aging and EPA also run HeatRisk.gov, which combines weather forecasts with medication risks. Over 1.2 million seniors used it in 2023. There’s even new research on supplements designed for seniors on multiple meds. Early trials show a blend of electrolytes and cooling agents improved thermoregulation by 28% in Phase 2 studies.Final Thought: Heat Is a Medical Emergency for Seniors on Meds
You can’t control the weather. But you can control how you respond to it. If you or a loved one is on any of these medications, don’t assume "I’ll be fine." Heat-related problems don’t announce themselves with sirens. They creep in quietly-through confusion, weakness, or a simple fall. Talk to your doctor now. Review your meds. Know the signs. Stay cool. It’s not just about comfort. It’s about survival.Can seniors stop taking diuretics during hot weather to avoid dehydration?
No. Stopping diuretics without medical supervision can be dangerous, especially for those with heart failure or high blood pressure. Instead, talk to your doctor about adjusting the dose or timing on hot days. You may need to drink more fluids or take electrolytes-but never change your meds on your own.
Is it safe for seniors to use fans during heat waves?
Fans only help if the air is cooler than your body. When temperatures hit 90°F or higher, fans just blow hot air around and can make things worse by increasing dehydration. Air conditioning is the only reliable way to cool down safely for seniors on heat-sensitive meds.
What should I do if my senior relative won’t drink water?
Try offering fluids they enjoy-broth, flavored electrolyte drinks, popsicles, or even water-rich fruits like watermelon and oranges. Set reminders every hour. Use a marked water bottle so they can see how much they’ve had. If they refuse fluids and show signs of confusion or dizziness, contact a doctor immediately.
Are over-the-counter meds like Benadryl safe in summer?
No. Diphenhydramine (found in Benadryl, Tylenol PM, and many sleep aids) blocks sweating and increases heat risk. Many seniors take it for allergies or sleep, not realizing the danger. Ask your pharmacist for a non-anticholinergic alternative like loratadine or cetirizine.
How do I know if my senior’s medication list is too risky for heat?
If they take two or more meds from these categories-diuretics, ACE inhibitors/ARBs, antipsychotics, or anticholinergics-they’re at higher risk. Use the CDC’s HM-RAT tool or ask a pharmacist to run a heat-risk check. A simple review can cut their risk by nearly 40%.