Personalized Pain Management Strategy Calculator
Step 1: Describe Your Pain
Step 2: Your Lifestyle Factors
For millions of people living with chronic pain, opioids used to be the go-to solution. But the risks - addiction, overdose, and long-term side effects - have made that path too dangerous. Today, the medical world has shifted. Non-opioid pain management isn’t just an option anymore; it’s the recommended first step. And the evidence shows it works.
Why Move Away From Opioids?
Opioids might ease pain quickly, but they don’t fix it. Studies show they offer little to no benefit for chronic pain after three months. Meanwhile, the dangers pile up: tolerance builds, doses creep higher, and the risk of dependence grows. In 2021, over 16,700 people in the U.S. died from prescription opioid overdoses. That’s not just a statistic - it’s a family, a friend, a neighbor. The CDC updated its guidelines in 2022 to make one thing crystal clear: non-opioid treatments should come first. For most types of chronic pain - back pain, osteoarthritis, nerve pain - non-opioid options work just as well, with far fewer risks.Non-Pharmacological Therapies That Actually Help
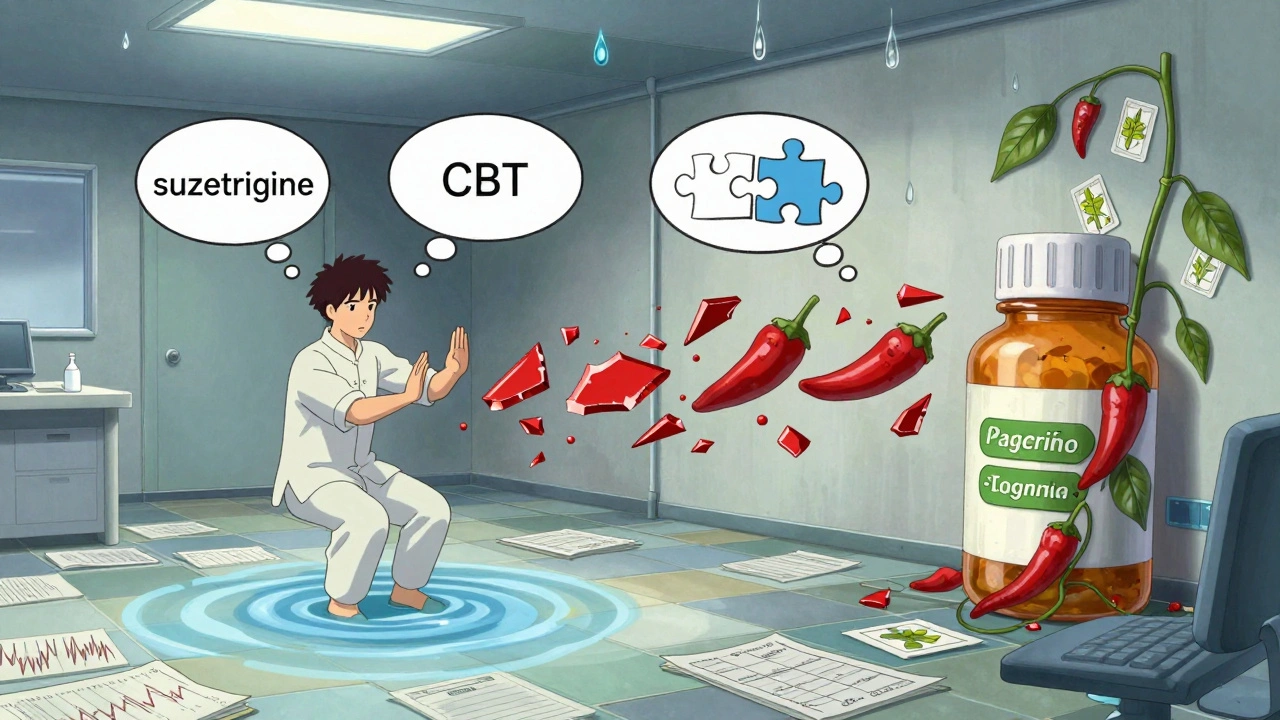
You don’t always need a pill to feel better. Some of the most effective pain relief comes from movement, mindset, and hands-on care.- Exercise therapy: Walking, swimming, or strength training just 2-3 times a week for 6-8 weeks can reduce pain and improve mobility. Physical therapists design these programs - they’re not just ‘do more steps.’
- Yoga, tai chi, and qigong: These mind-body practices combine gentle movement with breathing and focus. Research shows they reduce pain intensity and improve sleep in people with fibromyalgia and arthritis.
- Cognitive behavioral therapy (CBT): This isn’t talk therapy for depression. It’s a structured 8-12 session program that teaches you how your thoughts affect pain. People who complete CBT report less pain interference in daily life.
- Acupuncture: A 2022 survey of chronic pain patients found 52% got moderate to significant relief. It’s not magic - it likely triggers natural pain-relieving chemicals in the body.
- Massage and spinal manipulation: Especially helpful for lower back pain. One study showed massage was as effective as medication for short-term relief - without the stomach issues or drowsiness.
Non-Opioid Medications That Work
Sometimes, you need something stronger than movement. That’s where these medications come in - safe, proven, and widely used.- NSAIDs (ibuprofen, naproxen): Great for inflammation-based pain like arthritis. But long-term use can harm your kidneys or stomach. Stick to the lowest dose for the shortest time.
- Acetaminophen: Safe for most people if you don’t exceed 3,000-4,000 mg a day. Too much? Liver damage. It’s simple, but you need to track your intake - even if it’s in cold medicines too.
- Duloxetine and venlafaxine: These SNRI antidepressants are FDA-approved for chronic musculoskeletal pain and neuropathic pain. They don’t make you ‘happy’ - they change how your nerves send pain signals. It can take 4-6 weeks to feel the difference.
- Pregabalin and gabapentin: Used for nerve pain from diabetes, shingles, or sciatica. About 30-50% of users see meaningful relief. Side effects? Drowsiness, dizziness, and weight gain - common but manageable.
- Topical treatments: Capsaicin cream (from chili peppers) and lidocaine patches deliver pain relief right where it hurts. No stomach upset. No brain fog. Just targeted relief.
What Doesn’t Work as Well - and Why
Not every non-opioid option works for everyone. Some have limits.- NSAIDs: Not safe for people with kidney disease (15% of adults over 65 have this). Also risky if you have heart problems.
- Antidepressants: Take weeks to work. If you’re desperate for quick relief, they won’t help today.
- Physical therapy: You have to show up. Studies show only 30-70% of people stick with it long-term. Support matters.
- Acupuncture and massage: Insurance often limits coverage. You might pay out-of-pocket - $60-$120 per session.
Real People, Real Results
On Reddit’s r/ChronicPain community, one user shared how they cut their opioid use in half by combining aquatic therapy, CBT, and low-dose naltrexone. Another said yoga gave them back their mornings - no more pain pills before breakfast. But it’s not perfect. On Drugs.com, 45% of people who took NSAIDs reported stomach problems. Over 60% of pregabalin users said they felt drowsy. These aren’t side effects you ignore - they’re trade-offs you weigh. The key? Personalization. What works for someone with osteoarthritis might not help someone with nerve pain. There’s no one-size-fits-all.
How to Get Started
You don’t need to overhaul your life overnight. Start small.- Ask your doctor: ‘What non-opioid options are right for my type of pain?’
- Try one physical therapy session. Many clinics offer a free initial assessment.
- Download a free mindfulness app (like Insight Timer) and try 10 minutes a day for two weeks.
- Check your insurance: How many physical therapy or acupuncture visits do you get per year?
- Track your pain: Use a simple journal - rate your pain 1-10 daily. You’ll see patterns.