Levodopa Protein Timing Calculator
Optimize Your Protein for Better Levodopa Results
Your protein intake affects how well levodopa works. This tool helps you plan your protein distribution throughout the day to minimize 'off' periods.
Important Note: Protein blocks levodopa absorption when consumed simultaneously. For best results, follow the Protein Redistribution Diet (PRD) by shifting most protein to dinner.
Calculate Your Daily Protein Needs
Enter your body weight to determine your ideal daily protein intake. Recommended range: 0.6-0.8 grams per kilogram of body weight.
If you or someone you care about takes levodopa for Parkinson’s disease, eating a steak, chicken breast, or even a big bowl of beans might be making symptoms worse-not because of the food itself, but because of what’s inside it. Protein doesn’t just build muscle; it can block the medicine from working properly. This isn’t a myth or a vague warning. It’s a well-documented, biologically real conflict between food and medication that affects up to half of people on long-term levodopa therapy.
Why Protein Interferes with Levodopa
Levodopa is the gold-standard treatment for Parkinson’s. It’s the molecule your brain needs to make dopamine, the chemical that helps control movement. But levodopa doesn’t just walk into your brain. It has to fight its way through two major barriers: your gut and your blood-brain barrier. And at both points, it’s competing with something else-amino acids from the protein you eat. There are eight large neutral amino acids (LNAAs) that your body uses to build proteins: leucine, isoleucine, valine, phenylalanine, tyrosine, tryptophan, methionine, and histidine. These are the same amino acids that levodopa uses to get absorbed. They all share the same transporter system, called LAT1. When you eat a high-protein meal, your blood floods with these amino acids. Suddenly, levodopa is stuck in traffic. It can’t get through the gut wall as quickly, and even if it does, it struggles to cross into the brain. Studies show that after eating a meal with more than 10 grams of protein, levodopa absorption drops by 25-40%. The time it takes to reach peak levels in your blood can be delayed by up to 90 minutes. That means you might take your pill at 8 a.m., eat your scrambled eggs and bacon at 8:15, and not feel the medicine kick in until 10 a.m.-if it kicks in at all. The result? Unpredictable ‘off’ periods: sudden stiffness, slow movement, tremors returning-all because your brain didn’t get enough dopamine when it needed it.Who’s Most Affected?
Not everyone on levodopa runs into this problem. About 40-50% of people with Parkinson’s develop noticeable motor fluctuations linked to protein intake. But it doesn’t happen right away. It usually shows up after 8-13 years of taking levodopa, or when the disease has progressed to Hoehn & Yahr stages 3 or 4. That’s when the brain’s ability to store and release dopamine starts to fade, making you more dependent on each pill working perfectly. People who notice this interaction often describe it like this: “My meds work fine in the morning, but after lunch, I freeze up.” Or: “I can walk fine after my pill, but if I eat chicken with it, I’m stuck on the couch for hours.” These aren’t just bad days-they’re direct results of amino acid competition.Three Ways to Manage It
There are three main strategies doctors and dietitians use to fix this. None are perfect, but some work much better than others.1. Low-Protein Diet (LPD)
This approach cuts total daily protein to 0.6-0.8 grams per kilogram of body weight. For a 70kg person, that’s about 45-55 grams of protein per day-less than most people get in one meal. A typical day might include two eggs (12g), a small piece of fish (15g), and half a cup of lentils (7g). The rest of the calories come from carbs and fats. It sounds simple. But in practice, it’s tough. Many people lose weight unintentionally. One study found 31% of people on strict LPD lost over 5% of their body weight in six months. That’s dangerous for older adults, especially those already at risk for muscle loss. Plus, you miss out on important nutrients like vitamin B12 and iron, which are already low in 22% of long-term protein-restricted patients.2. Protein Redistribution Diet (PRD)
This is the most effective method-and the one most experts now recommend. Instead of cutting protein overall, you shift almost all of it to the evening meal. During the day, you eat very little protein-under 7 grams per meal. That means breakfast and lunch are mostly carbs, vegetables, fruits, and fats. Dinner is when you get your steak, beans, cheese, or tofu. Why does this work? Because levodopa is most needed during the day, when you’re moving, walking, and doing daily tasks. At night, you’re mostly sleeping. So even if protein blocks levodopa absorption in the evening, it doesn’t hurt your mobility as much. Research shows PRD reduces ‘off’ time by nearly two hours a day and adds about 30 minutes of smooth, controlled movement. One study found it was 35% more effective than a simple low-protein diet. And the success rate? Between 60% and 100% of people who try it see real improvement.3. Low-Protein Products (LPP)
These are specialty foods-low-protein bread, pasta, and flour-that let people eat more variety without hitting their protein limit. They help with adherence, but only slightly. Only 22% of users say they feel more satisfied with these products. They’re expensive, hard to find outside Europe and North America, and they don’t fix the core problem: you still have to plan every meal.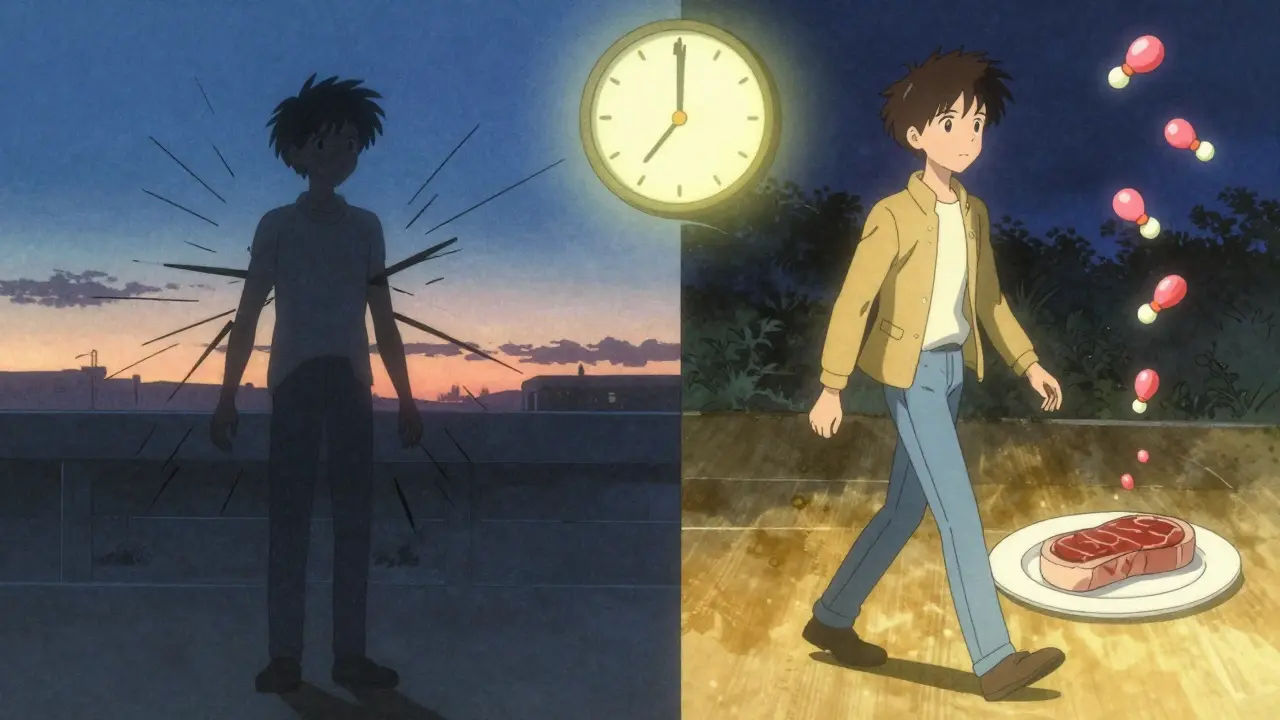
What About Timing?
Some people try taking levodopa 30-60 minutes before eating. It sounds logical. And for some, it works. But it’s not reliable. If your stomach empties slowly-which happens often in Parkinson’s-the pill might sit there for hours without being absorbed. Others find that taking it on an empty stomach causes nausea. One study showed effectiveness ranged from 30% to 65%, depending on the person. The best advice? Try it. Track your symptoms. If you take your pill at 7 a.m. and eat at 8 a.m., and you feel better than when you eat with your pill, keep doing it. If not, try PRD instead.Real-Life Challenges
This isn’t just a medical issue. It’s a social one. Families report strained dinners. Friends don’t understand why you can’t eat the lasagna. People skip events because they’re afraid of being stuck in an ‘off’ state. One Reddit user wrote: “I haven’t eaten at a restaurant in two years. Too many sauces, too much meat. I just don’t risk it.” And the hardest part? Adherence. Two out of three people quit strict protein plans within a year. Why? It’s boring. It’s isolating. It’s exhausting. But here’s the good news: when people work with a dietitian who customizes their plan-using their favorite foods, cultural dishes, and real-life routines-adherence jumps by 40%. One woman in Bristol switched from white rice and boiled chicken to curry with lentils and cauliflower rice. She kept it up for two years.What You Should Do
If you’re on levodopa and notice your symptoms getting worse after meals, don’t assume it’s your disease getting worse. It might be your plate. Start with a food and symptom diary. For one week, write down:- When you took your levodopa
- What you ate (and how much protein)
- How you felt 1-3 hours later (on, off, dyskinesia)

Who Should Avoid Protein Restriction?
Not everyone should do this. If you’re underweight (BMI under 20), have trouble swallowing, or are losing muscle, cutting protein could hurt you more than help. The same goes for people with other conditions like kidney disease or diabetes. Also, don’t assume you need it. Only 40-50% of people have a true protein-levodopa interaction. Some studies even show no change in levodopa levels with high-protein diets-suggesting the real issue might be at the blood-brain barrier, not the gut. That’s why personalized testing matters.The Future: Protein Pacing
There’s hope on the horizon. Researchers are testing something called “protein pacing”-giving tiny amounts of protein every few hours instead of big meals. Early trials show it keeps amino acid levels steady, so levodopa isn’t constantly blocked. So far, 68% of participants responded well, and adherence was much higher than with PRD. It’s still in Phase II trials, but it could change everything. Imagine eating a small portion of chicken with breakfast, a bit of tofu at lunch, and a little cheese at dinner-without any ‘off’ periods.Final Thought
This isn’t about giving up food. It’s about working smarter with what you eat. Protein isn’t the enemy. Levodopa isn’t weak. It’s just a system that evolved for natural eating patterns-not for pills and protein shakes. The goal isn’t perfection. It’s control. More good hours. Fewer frozen moments. Better nights. And yes-sometimes, that means eating your steak at 7 p.m. instead of 1 p.m. And that’s okay.Can I still eat meat if I take levodopa?
Yes, but timing matters. If you’re experiencing motor fluctuations, try moving meat and other high-protein foods to your evening meal. Avoid eating large portions of meat, dairy, eggs, or legumes within one hour before or after taking levodopa. Many people find success by eating protein only at dinner, leaving breakfast and lunch low in protein.
How much protein is too much when taking levodopa?
Consuming more than 10 grams of protein in a single meal can start to interfere with levodopa absorption. Meals with 20 grams or more can reduce bioavailability by up to 40%. For most people, keeping daytime meals under 7 grams of protein helps minimize interference. Total daily protein should be around 0.6-0.8 grams per kilogram of body weight, unless you’re underweight or advised otherwise by a doctor.
Does protein restriction cause weight loss?
Yes, if done too strictly. About 31% of people on low-protein diets lose more than 5% of their body weight in six months. This is especially risky for older adults with Parkinson’s, who are already prone to muscle loss. Always work with a dietitian to ensure you’re getting enough calories and nutrients. If you’re losing weight, your protein plan needs adjusting-not eliminating.
How long does it take to see results from a protein redistribution diet?
Most people notice improvements in motor control within 2-4 weeks. Some feel better in days, especially if they were previously eating protein with every dose. Full benefits-like reduced ‘off’ time and smoother movement-usually appear after 6-8 weeks. Consistency matters more than perfection. Even partial adherence can help.
Should I stop taking levodopa if I eat protein?
No. Never stop or change your levodopa dose without talking to your doctor. The goal is not to avoid protein entirely, but to manage when and how you eat it. Most people can still get enough protein by shifting it to the evening. Stopping levodopa can cause dangerous worsening of symptoms. Work with your care team to find a balance.
Are there any supplements that help with protein-levodopa interference?
Some studies have looked at large neutral amino acid supplements to compete with dietary amino acids, but results are mixed and not recommended without supervision. Instead, focus on timing and meal planning. Vitamin B12 and iron supplements may be needed if you’re on a long-term low-protein diet, since these nutrients are often found in protein-rich foods. Ask your doctor for blood tests to check for deficiencies.






