Vitamin D Deficiency in CKD: What You Need to Know
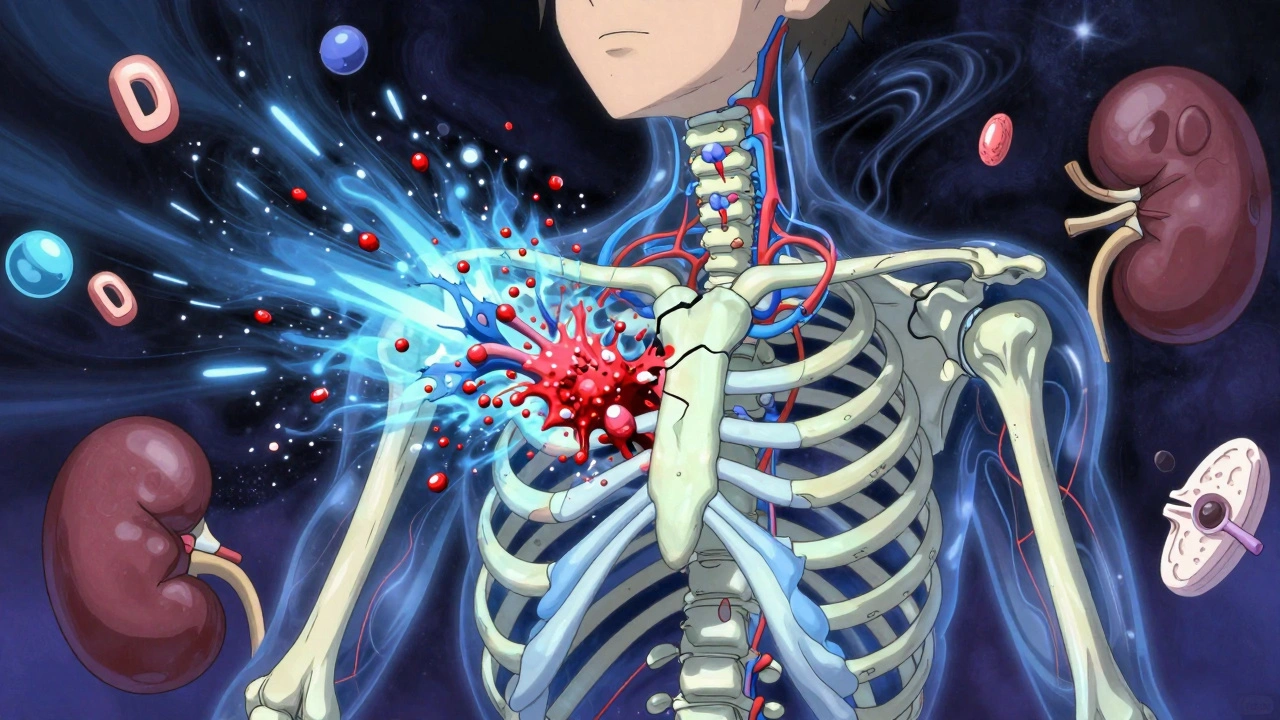
When your kidneys aren’t working right, your body struggles to turn vitamin D into its active form. This is a big reason why vitamin D deficiency, a condition where the body lacks enough active vitamin D to support bone, immune, and muscle health. Also known as calcitriol deficiency, it’s not just about weak bones—it’s linked to higher risks of heart problems, infections, and faster decline in chronic kidney disease, a long-term condition where kidney function drops over time, often due to diabetes or high blood pressure. About 80% of people with advanced CKD have low vitamin D levels, and it’s not always because they don’t get enough sun or eat enough dairy. The problem starts inside the kidneys themselves.
Your kidneys are the ones that convert vitamin D from food or sunlight into calcitriol, the version your body can actually use. When kidney damage hits, that conversion slows or stops. That’s why taking regular vitamin D supplements often doesn’t fix the issue. You need the active form—calcitriol or analogs like paricalcitol—which your doctor can prescribe. But here’s the catch: too much active vitamin D can raise calcium and phosphorus levels, which can damage your heart and blood vessels. That’s why testing is key. Doctors check 25-hydroxyvitamin D to see your overall levels, and 1,25-dihydroxyvitamin D to see if your body is making enough of the active kind. It’s not a one-size-fits-all fix.
People on dialysis are especially at risk. Their kidneys are nearly useless, and they often avoid sunlight or have dietary restrictions that limit vitamin D intake. Plus, many medications used for CKD—like phosphate binders or diuretics—can interfere with how vitamin D is absorbed or processed. This isn’t just a supplement issue. It’s a complex balance between bone health, heart safety, and kidney function. That’s why managing vitamin D in CKD isn’t about popping a pill. It’s about working with your care team to monitor levels, adjust treatment, and avoid hidden dangers.
What you’ll find below are real, practical posts from people who’ve lived with this, doctors who treat it, and studies that cut through the noise. You’ll see how vitamin D deficiency connects to muscle weakness, high blood pressure, and even depression in CKD patients. You’ll learn what lab results actually mean, why some supplements don’t help, and how to talk to your provider about the right kind of vitamin D. No fluff. No guesses. Just what works.