What Is CKD-Mineral and Bone Disorder?
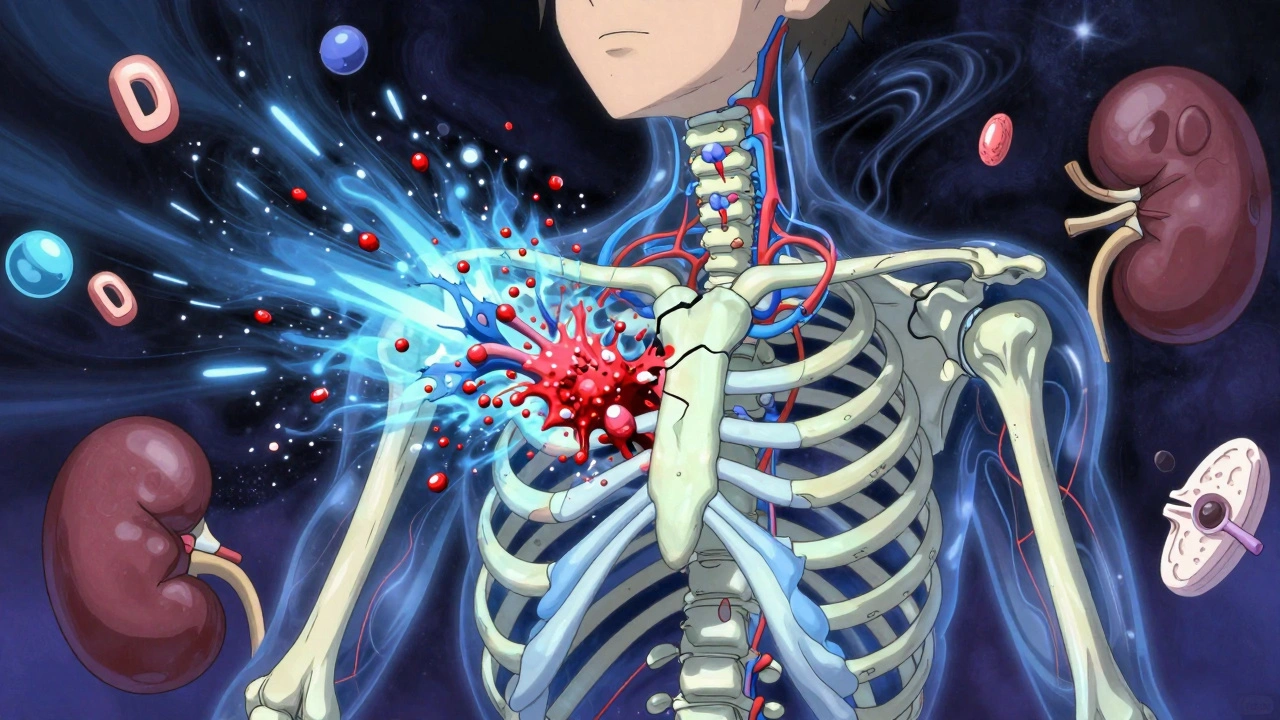
When your kidneys start to fail, they don’t just stop filtering waste-they also lose their ability to keep your bones and blood chemistry in balance. This isn’t just about weak bones. It’s a systemic problem called CKD-Mineral and Bone Disorder (CKD-MBD), a complex chain reaction involving calcium, phosphate, parathyroid hormone (PTH), and vitamin D. It affects nearly everyone with advanced kidney disease, and it’s one of the leading reasons people with kidney failure die from heart problems-not just kidney failure.
The Three-Part Problem: Calcium, PTH, and Vitamin D
Think of your body as a tightrope walker trying to keep three balls in the air: calcium, phosphate, and PTH. In healthy kidneys, these stay balanced. But when kidney function drops below 60 mL/min (Stage 3 CKD), the balance starts to collapse.
First, your kidneys can’t get rid of phosphate anymore. Phosphate builds up in your blood. That’s bad enough-but it triggers something worse. High phosphate makes your bones release calcium into your bloodstream. That sounds good, right? But then your body overcompensates.
Your parathyroid glands, tiny organs in your neck, sense low calcium and start pumping out too much PTH. This is called secondary hyperparathyroidism. PTH tries to fix the problem by pulling even more calcium from your bones. Over time, your bones become porous and fragile. At the same time, calcium and phosphate start sticking together in your blood vessels, turning them stiff and calcified-like rust inside your arteries.
And here’s the hidden player: vitamin D. Healthy kidneys convert vitamin D into its active form, calcitriol. But damaged kidneys can’t do this. Without enough active vitamin D, your gut can’t absorb calcium from food. Your calcium drops even more. Your PTH climbs higher. Your bones weaken. Your arteries harden. It’s a loop with no easy escape.
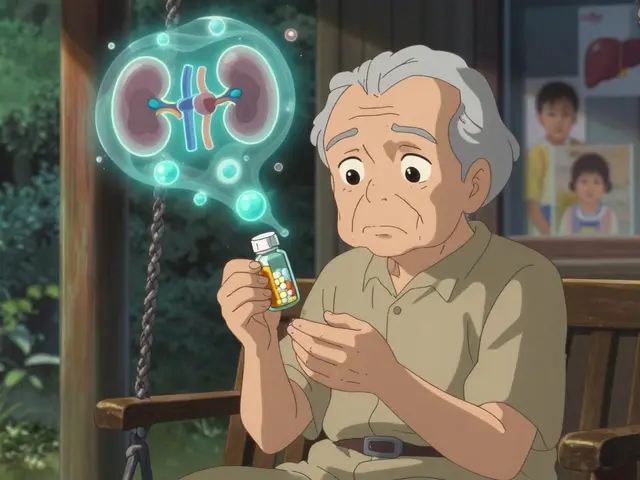
What the Numbers Mean
Doctors track four key numbers to see if CKD-MBD is worsening:
- Phosphate: Normal is 2.7-4.5 mg/dL. In Stage 5 CKD, it’s common to see levels above 5.5 mg/dL. Each 1 mg/dL rise above normal increases your risk of dying by 18%.
- PTH: Normal is 10-65 pg/mL. In advanced CKD, levels can hit 300-800 pg/mL or higher. But here’s the twist: even if PTH is sky-high, your bones might not respond. This is called ‘PTH resistance’-your body is screaming for help, but the signal isn’t getting through.
- Calcium: Target is 8.4-10.2 mg/dL. Too low? Bones break. Too high? Blood vessels calcify. It’s a tight line.
- Vitamin D (25-OH): Most people with CKD have levels below 20 ng/mL. The goal is at least 30 ng/mL. About 85% of dialysis patients are deficient.
These aren’t just lab values. They’re warning signs. A phosphate level over 5.5 mg/dL, combined with PTH over 500 pg/mL, means your bones are actively breaking down. If your calcium is high and phosphate is high, your arteries are likely calcifying faster than normal.
Bone Disease in CKD: It’s Not What You Think
For years, doctors called it ‘renal osteodystrophy.’ That term made people think of brittle, crumbling bones like in old age. But in CKD, bone disease looks different.
There are three main types:
- High turnover disease: Your bones are overactive. PTH is through the roof. Bone cells are working overtime, but they’re making weak, disorganized bone. This is the classic ‘osteitis fibrosa cystica.’ It’s rare now-seen in only 20-30% of dialysis patients.
- Low turnover disease (adynamic bone): This is the silent killer. PTH is low (under 150 pg/mL), and bone cells are barely active. Your bones don’t break down or rebuild. They just sit there, dense but brittle. Fractures happen without trauma. This affects 50-60% of dialysis patients today.
- Mixed disease: A bit of both. Often seen when treatment is inconsistent.
Here’s the scary part: a bone biopsy is the only way to know which type you have. But it’s invasive. So doctors guess based on PTH, calcium, and phosphate levels. That’s why so many people get the wrong treatment.
Vascular Calcification: The Silent Heart Killer
Most people don’t realize that CKD-MBD isn’t just a bone disease. It’s a heart disease.
Calcium and phosphate don’t just leak into your bones-they also deposit in your arteries. Coronary arteries, aorta, heart valves. By the time you’re on dialysis, 80-90% of patients have visible calcification on a CT scan. That’s 3-5 times higher than in people with healthy kidneys.
This calcification doesn’t cause chest pain like a clogged artery. It makes your arteries stiff. Your heart has to pump harder. Blood pressure spikes. The left side of your heart thickens. Eventually, it fails. In fact, cardiovascular disease causes half of all deaths in people with kidney failure.
And here’s the worst part: once calcification starts, it’s nearly impossible to reverse. Prevention is everything.
Treatment: It’s Not Just Pills
There’s no magic drug for CKD-MBD. Treatment is a three-pronged approach: diet, medication, and dialysis.
Diet: The First Line of Defense
Phosphate is everywhere-in processed foods, sodas, fast food, even bread. Your kidneys can’t handle it. So you have to cut back. Aim for 800-1,000 mg per day. That’s less than one can of cola (40 mg) and a slice of pizza (300 mg). It’s hard. But it’s necessary.
Phosphate Binders: The Necessary Evil
These pills stick to phosphate in your gut so it doesn’t get absorbed. Common ones:
- Calcium-based (calcium carbonate, acetate): Cheap and effective. But if you take too much, you get high calcium-and more calcification. Limit to 1,500 mg elemental calcium per day.
- Sevelamer (Renvela): Doesn’t raise calcium. Expensive, but safer for your arteries.
- Lanthanum (Fosrenol): Also calcium-free. Good for long-term use.
Aluminum-based binders? Avoid them. They cause brain damage over time.
Vitamin D: More Is Not Better
Don’t just take any vitamin D. If your 25(OH)D is below 30 ng/mL, take cholecalciferol (D3)-1,000 to 4,000 IU daily. It’s safe and lowers death risk by 15%.
But active forms like calcitriol or paricalcitol? Only use them if PTH is above 500 pg/mL. They raise calcium and phosphate. If you’re already high on those, they’ll make calcification worse.
Calcimimetics: The New Hope
Cinacalcet and etelcalcetide are drugs that trick your parathyroid glands into thinking calcium is higher than it is. They lower PTH without raising calcium or phosphate. Cinacalcet is taken daily. Etelcalcetide is an IV shot given after dialysis, three times a week. Both reduce PTH by 30-45% and are now first-line for severe hyperparathyroidism.
The Big Shift: Treat the Syndrome, Not Just the Numbers
For years, doctors chased perfect lab values. Lower phosphate. Lower PTH. Raise vitamin D. But studies show that pushing phosphate below 4.5 mg/dL can lead to malnutrition. Aggressively lowering PTH with surgery or drugs can cause adynamic bone disease.
The new approach? Balance. Target ranges, not extremes. KDIGO guidelines now say: aim for PTH 2-9 times the upper normal limit. Don’t panic if your phosphate is 5.2 mg/dL if you’re eating well and not gaining weight. Don’t rush to surgery if your PTH is 600 pg/mL but you’re not fracturing.
It’s not about hitting numbers. It’s about protecting your bones and your heart together.

What’s Coming Next?
Research is moving fast. New drugs are being tested:
- Anti-sclerostin antibodies (like romosozumab): These boost bone formation. Early trials show 30-40% increase in bone density in CKD patients.
- Klotho protein therapy: Klotho is a protein your kidneys make that helps remove phosphate. In CKD, Klotho drops. Animal studies show giving Klotho reduces calcification by 60%.
- FGF23 blockers: FGF23 rises early in CKD and drives vitamin D deficiency. Blocking it might stop the cascade before it starts.
One thing’s clear: the future of CKD-MBD isn’t just pills and dialysis. It’s precision medicine-tailoring treatment to your bone type, your calcification risk, your diet, your genetics.
What You Can Do Today
- Get your phosphate, calcium, PTH, and vitamin D checked every 3-6 months if you have Stage 3 or higher CKD.
- Ask your doctor: ‘Am I on a calcium-based binder? Is that safe for me?’
- Read food labels. Avoid ‘phosphate additives’-they’re in 70% of processed foods.
- Don’t take vitamin D supplements without knowing your 25(OH)D level.
- If you’re on dialysis, ask if you’re a candidate for etelcalcetide.
CKD-MBD isn’t a disease you can ignore. It’s a silent thief-stealing your bones, hardening your heart, and shortening your life. But it’s not unstoppable. With the right knowledge, the right treatment, and the right team, you can protect yourself.
Is CKD-MBD the same as osteoporosis?
No. Osteoporosis is bone loss due to aging or hormonal changes. CKD-MBD is caused by kidney failure and involves abnormal calcium, phosphate, and PTH levels. While both cause fractures, CKD-MBD also causes dangerous artery calcification, which osteoporosis does not.
Can vitamin D supplements cure CKD-MBD?
No. Nutritional vitamin D (cholecalciferol) helps if you’re deficient, but it doesn’t fix the core problem: your kidneys can’t activate it. Active forms like calcitriol can help lower PTH, but they raise calcium and phosphate-risking heart damage. They’re not a cure. They’re a tool, used carefully.
Why is phosphate so dangerous in CKD?
High phosphate directly triggers bone breakdown, suppresses active vitamin D, and causes calcium to deposit in blood vessels. Each 1 mg/dL increase in phosphate raises your risk of death by 18%. It’s not just a lab value-it’s a direct threat to your heart and bones.
Should I avoid dairy to lower phosphate?
Not necessarily. Dairy has calcium, which can bind phosphate in your gut. But it also contains phosphate. The key is balance. Choose low-phosphate dairy like fresh milk over processed cheeses. Pair dairy with phosphate binders if needed. Don’t eliminate it completely-you need calcium for your bones.
Can CKD-MBD be reversed?
Bone changes can improve with proper treatment-especially if caught early. But vascular calcification is mostly irreversible. That’s why prevention is critical. The goal isn’t reversal-it’s stopping further damage.
Do children with CKD get CKD-MBD too?
Yes-and it’s even more serious. In children, CKD-MBD can stunt growth, cause deformities, and delay puberty. By Stage 5, many are 1.5 to 2 standard deviations below normal height. Aggressive vitamin D and phosphate control are essential to protect their development.
Final Thoughts
CKD-MBD isn’t a single problem. It’s a cascade. One imbalance triggers another. And if you only treat one part, you’ll miss the bigger picture. The best outcomes come when your care team looks at your calcium, your PTH, your vitamin D, your diet, and your arteries-not as separate issues, but as one connected system.
Know your numbers. Ask questions. Don’t accept ‘normal’ labs if you’re still breaking bones or feeling worse. You have more control than you think.