Drug Metabolism Calculator
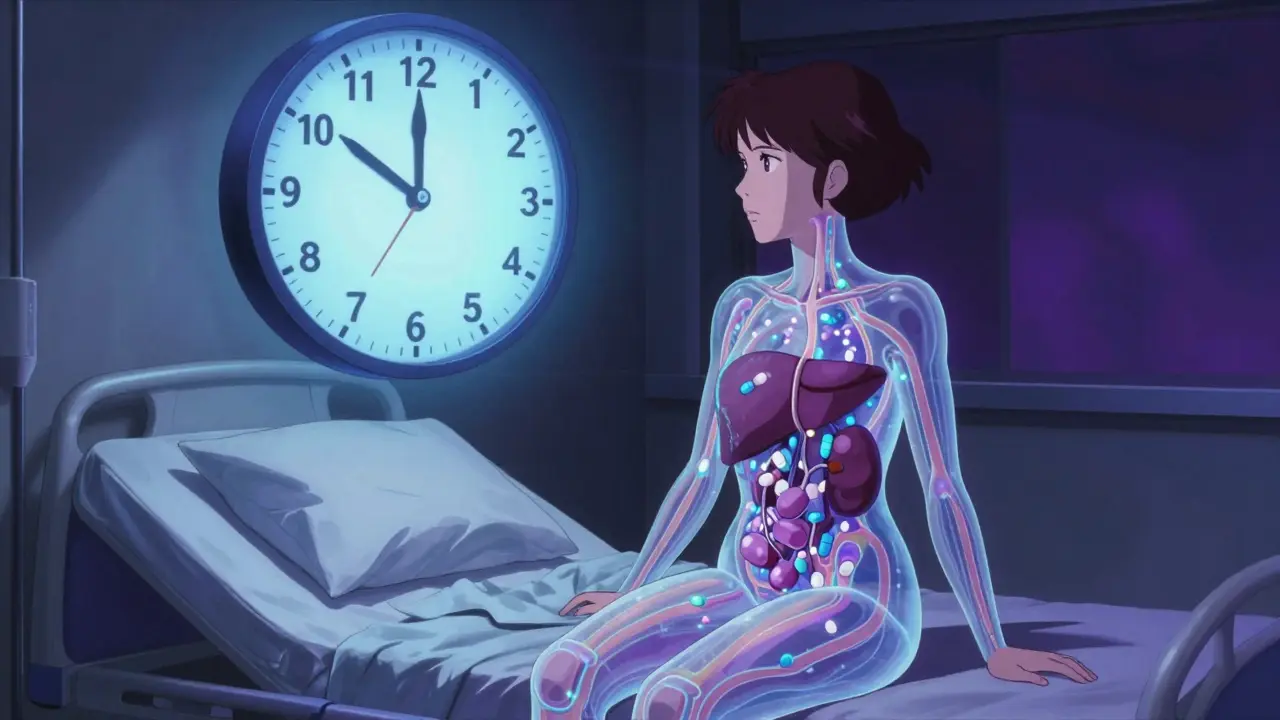
How Your Body Processes Medication
This calculator shows how biological differences between men and women can affect drug metabolism. Based on research from the article "Why Women Experience More Medication Side Effects Than Men".
Your Estimated Drug Processing
Based on research: Women metabolize drugs 40% slower due to lower CYP3A4 enzyme levels. Fat-soluble drugs stay 30% longer in women with higher body fat. Hormonal changes can alter metabolism by 30% during menstrual cycle.
Women are nearly twice as likely as men to have a bad reaction to the same dose of medication. It’s not just in their heads. It’s not because they’re more sensitive. It’s because most drugs were tested mostly on men - and women’s bodies process them differently.
Biological Differences That Change How Drugs Work
Your body doesn’t treat every drug the same way. And neither do men and women. Women generally have less of a key liver enzyme called CYP3A4 - about 40% less than men. This enzyme breaks down half of all prescription drugs, including common ones like statins for cholesterol and benzodiazepines for anxiety. Slower breakdown means the drug stays in the system longer, building up to levels that can cause dizziness, nausea, or even organ stress. Body composition plays a big role too. On average, women have 10-12% more body fat than men. Fat-soluble drugs like diazepam (Valium) get stored in fat tissue. That means women hold onto these drugs longer - up to 30% longer - leading to prolonged effects and higher risk of side effects. Kidneys also work differently. Women clear drugs like lithium and certain antibiotics 20-25% slower than men. Even small differences in weight, muscle mass, and hormone levels add up. Hormones shift everything. Oral contraceptives can make the body clear lamotrigine (used for epilepsy) 50-60% faster. That means a woman on birth control might need a higher dose to get the same effect. But during her menstrual cycle, her metabolism can swing up or down by 30% - meaning the same dose on day 5 might be too strong on day 20. No other group in medicine has to adjust their meds based on a monthly cycle - and yet, most prescriptions don’t account for it.Real-World Examples: Drugs That Hit Women Harder
Zolpidem (Ambien) is the clearest case. In 1992, researchers found women metabolized it 50% slower than men. But it took 21 years - until 2013 - for the FDA to act. They cut the recommended dose for women in half. After that, reports of next-day drowsiness, car accidents, and falls dropped by 38%. If this had happened in 1995, thousands of injuries could’ve been avoided. Digoxin, a heart drug, is another example. At the same dose, women have 20-30% higher blood levels. That increases their risk of dangerous heart rhythms by 40%. Yet, most doctors still prescribe the same dose to men and women. Antidepressants like sertraline and fluoxetine cause nausea and dizziness in women 1.5 to 2 times more often than men. Women also get QT prolongation - a heart rhythm issue - 2.3 times more often with antipsychotics like haloperidol. Meanwhile, men are more likely to suffer sexual side effects or urinary retention from anticholinergic drugs, but those rarely make headlines.Why This Gap Still Exists
The problem started in the 1970s. The FDA told drug companies to keep women out of early clinical trials - not because they thought women were different, but because they feared harm to unborn babies. So drug studies were done mostly on men. By the time a drug got approved, the dose was set based on male physiology. Even after the NIH Revitalization Act of 1993 required women to be included in trials, the fix wasn’t automatic. Researchers kept grouping men and women together in data analysis. A 2022 FDA review found only 12% of pharmacokinetic studies even looked at sex differences. That means for 88% of drugs, we still don’t know how women respond differently. Drug labels haven’t caught up. Out of 86 FDA-approved medications with known sex-based differences, only 4% have sex-specific dosing instructions. That’s not because doctors are ignoring the science - it’s because the science isn’t clearly labeled. A 2022 AMA survey found 67% of physicians didn’t even know about the zolpidem dose change for women.
Are Biological Differences the Whole Story?
Some experts say biology isn’t the only factor. Sarah Richardson at Harvard analyzed 33 million FDA adverse event reports and found that when you account for the fact that women take 56% more prescriptions than men, the difference in adverse reactions drops to less than 5%. That suggests part of the problem is exposure - women just take more meds. There’s also reporting bias. Women are more likely to notice symptoms, talk to their doctors, and report side effects. Men often tough it out or dismiss dizziness or nausea as "just stress." That doesn’t mean the biological differences aren’t real - they are. But it means we’re seeing a mix of biology and behavior. Janine Austin Clayton from the NIH puts it plainly: "Biological differences exist. But so does the way we ask questions and collect data. We’ve been looking at women through a male lens."What’s Being Done - and What’s Not
There are signs of progress. The European Medicines Agency now requires sex-stratified data in all Phase III trials. The FDA launched its "Sex and Gender Roadmap" in 2023, aiming to make sex a standard part of drug review by 2026. The NIH is funding a $12.5 million center at Harvard to study sex differences in medicine. But adoption is slow. In 2023, 78% of new cancer trials tracked sex differences - but only 32% of heart drug trials did. And while companies like Adyn and Womb Society are building drugs specifically for women, they’re still less than 0.5% of total pharmaceutical R&D. The biggest barrier? Time. It takes 10-15 years to change dosing guidelines after new evidence emerges. The zolpidem case proves that. The science was clear in 1992. The fix didn’t come until 2013. What other drugs are we still dosing wrong?