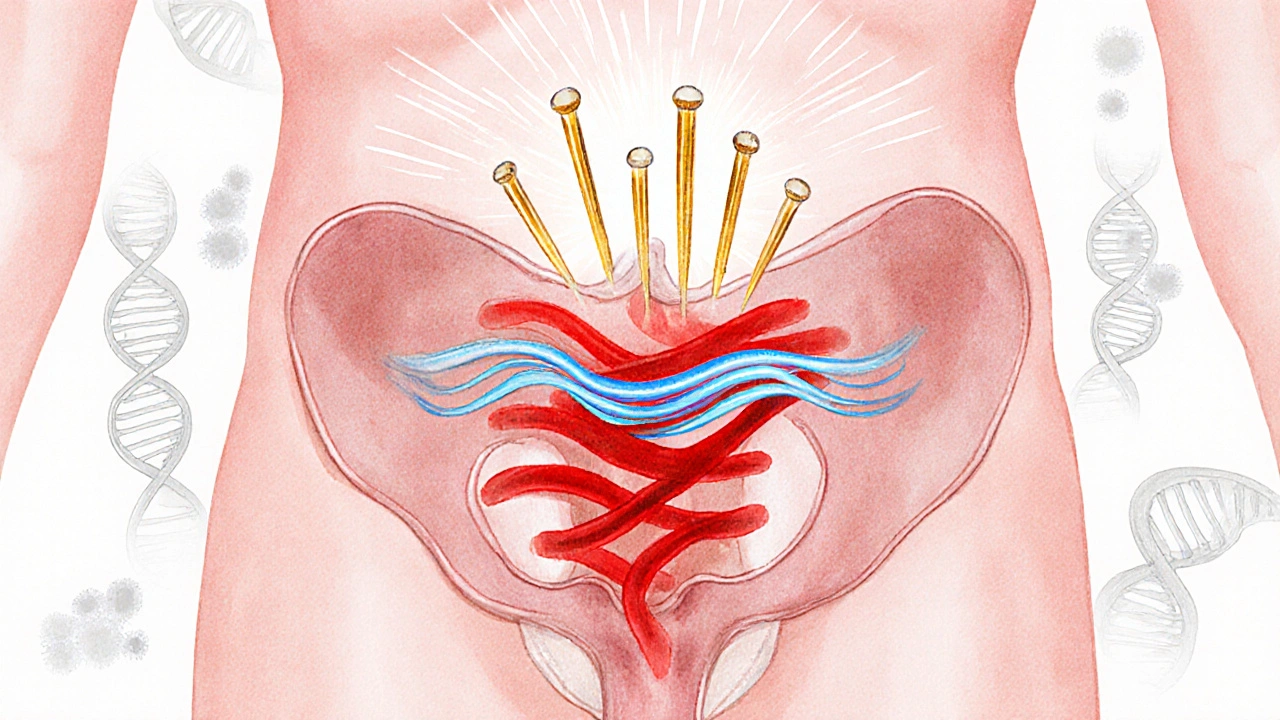
Acupuncture is a needle‑based therapy rooted in Traditional Chinese Medicine (TCM) that stimulates specific points on the body to balance the flow of Qi (energy) and promote healing. When applied to urinary issues, it targets the bladder meridian and surrounding pelvic structures, offering a drug‑free option for people plagued by painful bladder spasms.
Understanding Bladder Spasms
Bladder spasm is a sudden, involuntary contraction of the detrusor muscle that often causes urgency, frequency, and sometimes pain. The condition can stem from overactive bladder syndrome, urinary tract infections, or irritation after surgery. Typical symptoms include a sudden urge to urinate, leakage, and a feeling of incomplete emptying.
Why Acupuncture Makes Sense for This Problem
Acupuncture’s core premise is that health depends on a smooth flow of Qi through a network of Meridians - invisible pathways that link organs and tissues. The bladder meridian runs along the back of the leg and up the spine, intersecting the pelvic floor muscles that control bladder contraction. By inserting fine needles at strategic points, a practitioner can:
- Modulate nerve signals that trigger detrusor overactivity.
- Promote release of endogenous opioids, reducing pain associated with spasms.
- Improve local blood circulation, aiding tissue recovery.
Electroacupuncture, a variant that adds a mild electric current to the needles, has shown stronger effects on muscle relaxation, making it a popular choice for urological complaints.
Clinical Evidence: What the Studies Say
Randomised controlled trials (RCTs) from the past decade provide a growing evidence base:
- In a 2022 Chinese study involving 120 participants with overactive bladder, 8‑week electroacupuncture reduced daytime frequency by an average of 3.2 episodes per day (p<0.01) compared to sham treatment.
- A 2023 UK pilot trial on 45 patients reported a 45% improvement in urgency scores after a 6‑session acupuncture course, with no serious adverse events.
- Meta‑analysis of 9 RCTs (over 800 participants) concluded that acupuncture lowered the International Prostate Symptom Score (IPSS) by 2.7 points on average, outperforming placebo and matching the efficacy of first‑line anticholinergic drugs.
Safety data are reassuring: mild bruising or temporary soreness occurs in < 5% of cases, and there are no reported systemic side‑effects.
How Acupuncture Stacks Up Against Conventional Options
| Treatment | Typical Effectiveness (% symptom relief) |
Side‑Effect Profile | Invasiveness |
|---|---|---|---|
| Acupuncture | 40‑60 | Mild bruising, rare infection | Low (needle insertion) |
| NSAIDs | 20‑35 | Gastro‑intestinal upset, renal risk | Oral |
| Biofeedback Therapy | 30‑50 | None reported | Medium (electrode pads) |
| Anticholinergic Drugs | 45‑65 | Dry mouth, constipation, cognitive fog | Oral |
While drug therapies can yield comparable relief, they often bring systemic side‑effects that many patients wish to avoid. Acupuncture offers a middle ground: moderate effectiveness with a gentle safety profile.
What to Expect in an Acupuncture Course
A typical regimen for bladder spasms follows these steps:
- Initial consultation: The practitioner records medical history, evaluates bladder symptoms (using tools like the Overactive Bladder Symptom Score), and selects points on the Pelvic floor muscle and bladder meridian.
- Needle placement: 6‑8 ultra‑thin needles are inserted 15‑30 minutes, sometimes connected to a low‑frequency electro‑stimulator.
- Session frequency: 1-2 sessions per week for 4‑6 weeks, followed by a maintenance phase based on symptom response.
- Post‑session care: Light stretching, adequate hydration, and a bladder diary to track progress.
Most patients notice a gradual reduction in urgency after 2‑3 sessions. It’s crucial to continue the diary; the data often guide whether additional sessions are needed.
Safety, Contra‑indications, and Frequently Overlooked Details
Acupuncture is generally safe, but certain conditions require caution:
- Bleeding disorders or anticoagulant therapy - risk of bruising.
- Pregnancy - some points are avoided to prevent uterine stimulation.
- Severe infections near the insertion site - defer treatment until cleared.
Choosing a certified practitioner (registered with the British Acupuncture Council) reduces the likelihood of infection. Sterile, single‑use needles are mandatory.
Related Concepts and Next Steps in the Knowledge Cluster
Acupuncture sits within a broader Traditional Chinese Medicine framework that includes herbal formulas, dietary advice, and Qi‑gong exercises. For readers interested in a holistic approach, consider exploring:
- Herbal blends that strengthen the kidney and bladder energetics.
- Pelvic floor physiotherapy - a Western counterpart that works on muscle tone.
- Urodynamic testing - objective measurement of bladder pressure, useful for complex cases.
- Mind‑body techniques like mindfulness, which can modulate the stress component that often worsens overactivity.
Each of these topics expands the conversation from a single modality to a comprehensive bladder‑health strategy.
Frequently Asked Questions
Is acupuncture painful for bladder spasm patients?
The needles are extremely fine (about the thickness of a human hair). Most people feel a slight tingling or heaviness at the insertion point, but not pain. Any discomfort usually fades within a few minutes after the needles are placed.
How many sessions of acupuncture are needed to see improvement?
Clinical trials report noticeable reductions in urgency after 2‑3 sessions, with optimal results after 6‑12 visits. The exact number depends on severity, personal response, and consistency of treatment.
Can I combine acupuncture with medication?
Yes. Acupuncture is often used as an adjunct to anticholinergic drugs or beta‑3 agonists. Always discuss any combination with your urologist to avoid unexpected interactions.
Are there any risks specific to bladder health?
Serious complications are rare. The primary concerns are local infection (prevented by sterile needles) and fainting, which is uncommon. No evidence suggests acupuncture worsens bladder function.
What’s the difference between regular acupuncture and electroacupuncture?
Electroacupuncture adds a low‑frequency electric current to the needles, enhancing muscle relaxation and nerve modulation. It’s frequently chosen for pelvic‑floor related issues because the stimulation can reach deeper tissues.
Do insurance plans cover acupuncture for bladder spasms?
Coverage varies across the UK. Some NHS trusts offer acupuncture as part of chronic pain pathways, while private insurers may require a referral. Check your policy or ask the clinic’s admin staff for details.
How can I find a qualified practitioner?
Look for registration with the British Acupuncture Council (BAcC) or the General Acupuncture Council (GAcC). Qualified therapists have completed at least a 3‑year diploma and adhere to strict hygiene standards.
Will acupuncture cure my bladder spasms permanently?
Acupuncture can significantly reduce symptom frequency and severity, but long‑term remission often requires lifestyle adjustments, pelvic‑floor exercises, and, occasionally, maintenance sessions.






