Every year, medication adherence fails for millions of Americans-not because they don’t want to get better, but because they can’t afford to take their pills. Skipping a dose because the co-pay is $80. Splitting a $500 insulin pen in half to make it last. Delaying a refill until next paycheck. These aren’t rare stories. They’re daily realities for 1 in 5 adults in the U.S. who skip, cut, or delay meds because of cost. And the consequences? Deadly. Around 125,000 people die each year in the U.S. because they didn’t take their medicines as prescribed. That’s more than traffic accidents or gun violence. This isn’t just a personal struggle-it’s a systemic crisis.
Why Cost Stops People from Taking Their Meds
It’s not just about high list prices. It’s how the system is built. Even if you have insurance, you might still pay hundreds a month out of pocket. Deductibles, coinsurance, tiered formularies, and surprise pharmacy bills all add up. A study in the American Journal of Managed Care found that when co-pays jumped from $10 to over $50, adherence dropped by 15-20%. For someone on multiple chronic meds-say, blood pressure, diabetes, and cholesterol-that can mean $300-$600 a month just to stay alive. People with heart disease are especially vulnerable. Research shows they’re more likely to skip meds when costs rise than those with cancer or diabetes. Why? Because many heart meds are older, off-patent drugs that don’t have patient assistance programs. And unlike insulin, which got headlines, drugs like metoprolol or lisinopril rarely make the news-even though they’re just as essential. Then there’s the “sticker shock” factor. A 2022 survey found that 41% of patients were shocked by the final price at the pharmacy, even after their doctor said the drug was “covered.” That’s because insurance formularies change without warning, and pharmacies don’t always update prices in real time. You walk in thinking you’ll pay $15. You leave owing $120. That kind of betrayal makes people stop trusting the system-and their prescriptions.Who Gets Hit the Hardest
Cost-related nonadherence doesn’t affect everyone equally. Low-income individuals, especially those earning under $25,000 a year, are 3.2 times more likely to skip meds than those making over $75,000. Women, Black and Hispanic patients, and younger adults under 45 report higher rates of rationing pills. Why? They’re more likely to be juggling rent, childcare, food, and transportation-and meds are often the first thing to go. Even Medicare beneficiaries aren’t safe. In 2022, 18% of all U.S. adults said they didn’t fill a prescription because of cost. Among seniors on Medicare Part D, 14.4% reported cutting back on meds due to price. One 62-year-old woman in a Kaiser Health News interview said she pays $350 a month for her meds after insurance. She chooses between her prescriptions and groceries. That’s not a choice anyone should have to make.Real People, Real Stories
On Reddit, r/healthcare and r/Medicare are full of posts like this: “I take 5 meds. My co-pays total $800/month. I’m on disability. I’ve started splitting my 10mg pills in half to make them last.” Another user wrote: “My insulin used to be $130. Now it’s $420. I’m using a 10-year-old pump because I can’t afford a new one.” These aren’t outliers. They’re symptoms of a broken system. But there are also success stories. One type 2 diabetes patient in a case study from the American Diabetes Association was paying $500 a month for insulin. After enrolling in her manufacturer’s patient assistance program, her cost dropped to $25. Her adherence jumped from 60% to 95%. That’s the power of help-if you know where to look.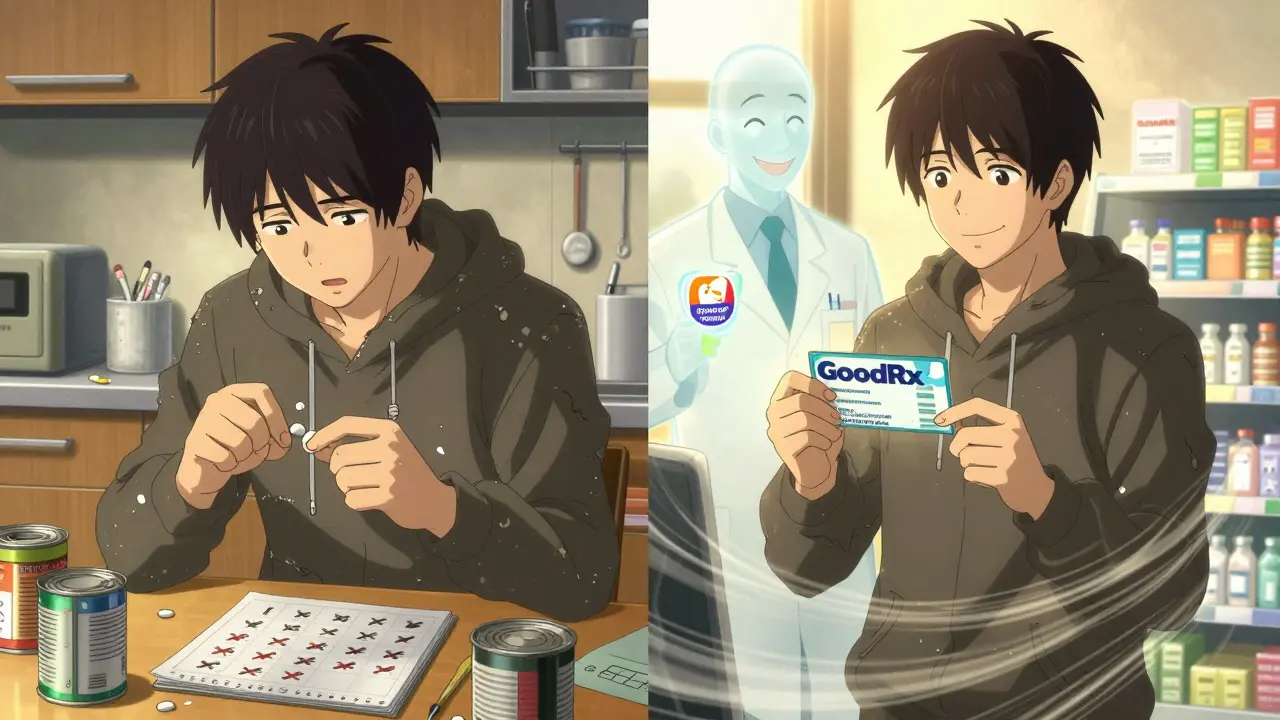
How to Get Help: Practical Steps You Can Take Today
You don’t have to choose between your health and your rent. Here’s what actually works:- Ask your doctor for alternatives. Not every drug on your script is the only option. Your doctor can check if there’s a generic, a lower-tier drug, or one covered by your insurance. The American Medical Association says doctors should always check formulary alignment before prescribing.
- Use GoodRx or SingleCare. These apps compare prices across pharmacies and often cut costs by 50-80%. In 2023, over 35 million Americans used them monthly. You don’t need insurance to use them. Just show the coupon at the counter.
- Apply for patient assistance programs. Pharmaceutical companies run these for people with low income. Most require income under 400% of the federal poverty level ($55,520 for one person in 2023). Programs like Patient Services Inc. helped 1.8 million people in 2022. You can apply online in minutes.
- Ask for a 90-day supply. Many insurers charge less per pill for 90-day fills. Mail-order pharmacies often offer this at 20-30% lower cost than 30-day refills. It’s one less trip to the pharmacy and one less bill to worry about.
- Check if you qualify for Medicare Extra Help. If you’re on Medicare and have limited income, this program can cover up to $5,000 in annual drug costs. Apply through Social Security.
- Use the Partnership for Prescription Assistance. This nonprofit connects you to over 475 programs from 450+ companies. Just call or visit their website-they do the legwork for you.
What’s Changing in 2025 and Beyond
There’s real hope on the horizon. The Inflation Reduction Act is reshaping how seniors pay for drugs. Starting in 2025, Medicare Part D will cap out-of-pocket spending at $2,000 a year. The infamous “donut hole” is gone. And for the first time, beneficiaries can pay for high-cost meds in monthly installments instead of one big bill. The FDA approved 1,123 generic drugs in 2022 alone, driving down prices for off-patent meds. More insurers are using real-time benefit tools that show you the exact price before you leave the doctor’s office. But here’s the catch: 37% of those estimates still don’t match what you pay at the pharmacy. So don’t rely on them alone. Still, experts warn: without structural changes to drug pricing, cost-related nonadherence will keep rising. The Congressional Budget Office projects U.S. drug spending will hit $1.1 trillion by 2031. That’s more than double what it was in 2022. And unless prices are capped, more people will keep choosing between food and pills.
What to Say to Your Doctor
Talking about money with your doctor can feel awkward. But it’s your right. You’re not being rude-you’re being smart. Try these phrases:- “I’m having trouble affording this prescription. Is there a cheaper option?”
- “Can we check if this drug is on my insurance’s formulary?”
- “Do you have samples I can try?”
- “Is there a patient assistance program for this medicine?”
Final Thought: You’re Not Alone
Medication adherence isn’t about willpower. It’s about access. The system is designed to make you feel like you’re failing when you can’t afford your meds. But the truth? The system is failing you. You don’t have to suffer in silence. You don’t have to ration your pills. There are real, working solutions-and they’re not just for the rich. The tools are out there. You just need to ask, apply, and advocate.Take one step today. Call your pharmacy. Check GoodRx. Ask your doctor. Reach out to a patient assistance program. One small action can mean the difference between survival and decline.
Why do people skip doses because of cost?
People skip doses because out-of-pocket costs for prescriptions can be unaffordable-even with insurance. High co-pays, deductibles, and tiered drug lists mean some patients pay hundreds a month. When faced with choices like paying for meds, rent, or groceries, many choose to cut back on pills to make ends meet. Studies show that when co-pays exceed $50, adherence drops by 15-20%.
Can I get help if I have Medicare?
Yes. Medicare beneficiaries can apply for the Extra Help program, which reduces Part D costs for low-income individuals. In 2023, it covers up to $5,000 in annual drug expenses. Starting in 2025, Medicare will also cap out-of-pocket drug spending at $2,000 per year and eliminate the coverage gap. You can apply through Social Security or your state’s Medicaid office.
Do generic drugs work as well as brand-name ones?
Yes. Generic drugs contain the same active ingredients, dosages, and safety profiles as brand-name versions. The FDA requires them to meet the same standards. Generics often cost 80-85% less. In 2022, the FDA approved over 1,100 new generics, making more affordable options available. Ask your doctor if a generic version of your prescription is available.
How do GoodRx and SingleCare work?
GoodRx and SingleCare are free price-comparison tools that show you the lowest cash price for your prescription at nearby pharmacies. You don’t need insurance. Just search your drug, pick the best price, and show the coupon at the pharmacy. These tools can cut costs by 50-80%. In 2023, over 35 million Americans used them monthly.
What if my doctor won’t change my prescription?
If your doctor says no, ask for a second opinion or ask to speak with a pharmacist at your pharmacy. Many pharmacies have clinical pharmacists who can suggest lower-cost alternatives or help you apply for patient assistance programs. You can also contact Patient Services Inc. or the Partnership for Prescription Assistance-they work directly with providers to find solutions.
Are patient assistance programs hard to qualify for?
Not usually. Most programs require income under 400% of the federal poverty level-which is $55,520 for a single person in 2023. Many don’t require proof of insurance. You’ll need basic info like your income, prescription details, and doctor’s name. Applications are free and can be completed online in under 15 minutes. Over 1.8 million Americans got help through these programs in 2022.
Is it safe to split pills to save money?
Some pills can be safely split, but not all. Extended-release, coated, or capsule-form medications should never be split-they can become unsafe or ineffective. Always ask your pharmacist before splitting any pill. If you’re considering this, talk to your doctor about switching to a lower-strength tablet instead.
Next Steps: What to Do Right Now
If you’re struggling to afford your meds, start here:- Write down all your prescriptions, dosages, and current monthly costs.
- Go to GoodRx.com or SingleCare.com and search each drug. Note the lowest cash price.
- Call your pharmacy and ask if they accept those coupons.
- Ask your doctor: “Is there a cheaper alternative or a generic?”
- Visit needymeds.org or ppa.org to check eligibility for patient assistance programs.
- If you’re on Medicare, call 1-800-MEDICARE to ask about Extra Help.
You don’t need to wait for policy changes to get help. The tools are here. The programs exist. And you deserve to take your medicine without choosing between your health and your rent.