When you have diabetes, your kidneys are under constant stress. Over time, high blood sugar damages the tiny filters in your kidneys, causing them to leak protein into your urine. This condition is called diabetic nephropathy, and it’s the leading cause of kidney failure in people with diabetes. But here’s the good news: two types of blood pressure medications - ACE inhibitors and ARBs - can slow or even stop this damage. And the key isn’t just lowering blood pressure. It’s reducing protein leakage. That’s where the real protection comes from.
What Exactly Is Diabetic Nephropathy?
Diabetic nephropathy isn’t just about high blood sugar. It’s about how that sugar slowly destroys the glomeruli - the filtering units in your kidneys. When these filters break down, they start letting albumin, a type of protein, escape into your urine. Doctors call this albuminuria. If you have more than 30 mg of albumin per gram of creatinine in your urine for three months or longer, you’re diagnosed with diabetic nephropathy. This isn’t just a lab result. It’s a warning sign that your kidneys are failing, and your heart is at risk too. People with this condition are far more likely to have heart attacks, strokes, or die from cardiovascular disease.
It doesn’t matter if you have type 1 or type 2 diabetes. If your blood sugar stays high over years, your kidneys pay the price. The earlier you catch it, the better your chances of stopping it. That’s why annual urine tests for albumin are part of standard diabetes care. If your doctor hasn’t checked your urine for protein in the last year, ask for it.
Why ACE Inhibitors and ARBs Are First-Line Treatment
For over 20 years, ACE inhibitors and ARBs have been the go-to medications for diabetic nephropathy. Why? Because they do something no other blood pressure pills can: they reduce protein leakage directly, even when blood pressure is already normal.
ACE inhibitors (like captopril, ramipril, benazepril) block the enzyme that turns angiotensin I into angiotensin II - a powerful chemical that tightens blood vessels and raises pressure inside the kidneys. ARBs (like losartan, irbesartan, valsartan) block the receptors that angiotensin II binds to. Both actions lower the pressure inside the kidney’s filtering units. Less pressure means less protein leaks out.
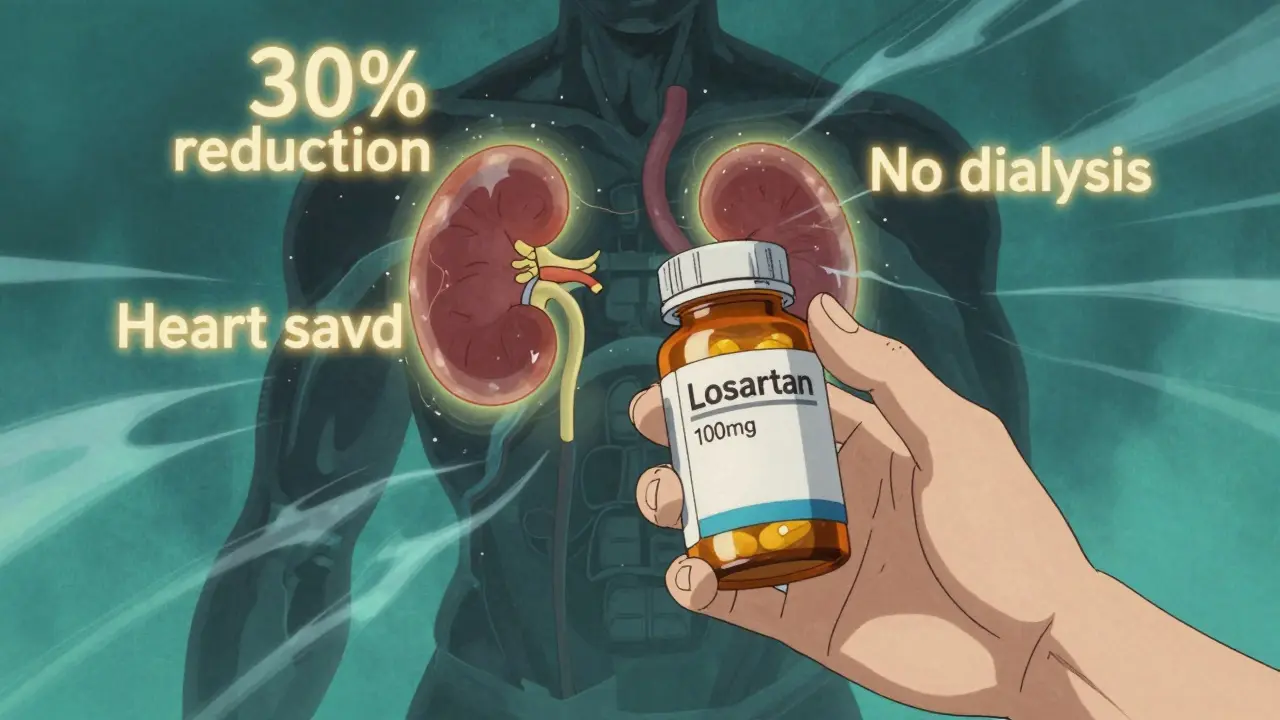
Large studies prove this works. The RENAAL trial showed that losartan reduced the risk of kidney failure by 28% in people with type 2 diabetes and heavy proteinuria. The IDNT trial found similar results with irbesartan. These weren’t small effects. These were life-changing outcomes - fewer people needed dialysis or kidney transplants.
And it’s not just about advanced disease. Even if you have early signs of kidney damage - microalbuminuria - starting an ACE inhibitor or ARB can reverse it. One study found that 30% of patients with early diabetic nephropathy saw their urine protein levels drop back to normal after six months on these drugs.
Dosing Matters More Than You Think
Here’s where most doctors and patients get it wrong. Many start with a low dose - 5 mg of ramipril, 25 mg of captopril - and never increase it. But clinical trials that proved these drugs work used maximum tolerated doses. That means 20 mg of ramipril, 50 mg of captopril three times a day, or 100 mg of losartan.
Low doses help with blood pressure. But only high doses protect your kidneys. The American Diabetes Association’s 2025 guidelines say clearly: if you’re on an ACE inhibitor or ARB for diabetic nephropathy, you must be on the highest dose your body can handle. If you’re not, you’re not getting the full benefit.
And don’t panic if your creatinine rises a little. A 20-30% increase in serum creatinine after starting one of these drugs is normal. It’s not kidney damage - it’s the drug doing its job. The kidneys are relaxing their filters, which lowers pressure and reduces protein leakage. That slight rise in creatinine means the medication is working. Stopping the drug because of this is one of the biggest mistakes in diabetes care.
What About Combination Therapy?
You might think: if one ACE inhibitor or ARB helps, two must help more. That’s logical - but it’s wrong.
Studies like VA NEPHRON-D, ONTARGET, and ALTITUDE tested combining ACE inhibitors with ARBs, or adding a direct renin inhibitor. The results were clear: no extra kidney protection. But the risks went way up. Patients had twice the chance of dangerously high potassium levels (hyperkalemia). They were also twice as likely to suffer sudden kidney failure.
Don’t combine them. Ever. Not even if your doctor suggests it. The guidelines from KDIGO, ADA, and the American Academy of Family Physicians all say the same thing: use one or the other - but not both.
Other Medications You Might Need
ACE inhibitors and ARBs are the foundation - but they’re not the whole house. Most people with diabetic nephropathy also need other blood pressure drugs to reach their target (usually under 130/80 mmHg).
Diuretics like furosemide help remove extra fluid. Calcium channel blockers like amlodipine relax blood vessels. Beta blockers like metoprolol can help if you have heart issues. But here’s the rule: these are add-ons. Never replacements. If you’re on a diuretic or calcium channel blocker alone, you’re missing the kidney protection that ACE inhibitors and ARBs provide.
And watch out for NSAIDs - ibuprofen, naproxen, celecoxib. These painkillers can suddenly wreck kidney function in people with diabetic nephropathy, especially when taken with ACE inhibitors or ARBs. If you need pain relief, talk to your doctor. Acetaminophen is usually safer.
The New Players: SGLT2 Inhibitors and MRAs
In the last five years, two new classes of drugs have changed the game: SGLT2 inhibitors (like empagliflozin, dapagliflozin) and nonsteroidal mineralocorticoid receptor antagonists (like finerenone).
These drugs also protect the kidneys - even more than ACE inhibitors and ARBs in some cases. But here’s the catch: every major trial that proved their benefit did so in patients who were already on a maximally tolerated ACE inhibitor or ARB. That means these new drugs work best on top of the old standard.
If you can’t tolerate an ACE inhibitor or ARB - maybe you get a dry cough or your potassium spikes - then SGLT2 inhibitors become your first choice. But if you can take them, don’t skip them. They’re part of the new standard of care.
What About Prevention?
Should everyone with diabetes take an ACE inhibitor or ARB to prevent kidney damage? No.
Studies show no benefit for people with normal blood pressure and no protein in their urine. Giving these drugs to someone with perfectly healthy kidneys doesn’t stop damage - it just raises the risk of side effects. The NIH and ADA both say: don’t use them for primary prevention.
Only start them if you have high blood pressure, protein in your urine, or both. That’s the trigger. That’s when the benefit outweighs the risk.
Why So Many People Are Still Not Getting Treated
Despite all the evidence, only 60-70% of people with diabetic nephropathy are actually on an ACE inhibitor or ARB. Why?
Some doctors fear the creatinine rise. Some patients stop because they feel dizzy or get a cough. Others just don’t know they need it. But the truth is simple: if you have diabetes and kidney damage, not taking one of these drugs is suboptimal care. It’s not just a recommendation - it’s the standard.
And if your doctor isn’t pushing you to the highest tolerated dose, ask why. You deserve the full benefit.
Protein Control: The Hidden Key
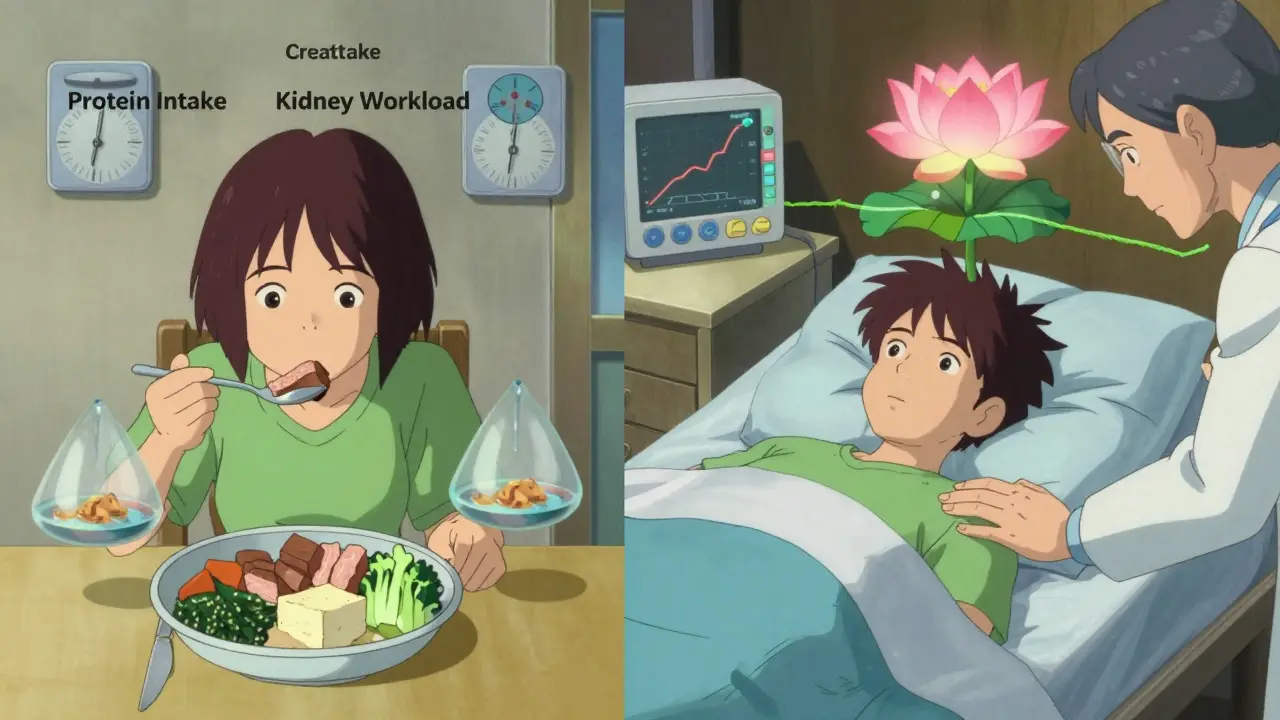
There’s one more piece: diet. While medication does the heavy lifting, reducing protein intake can help too. Most guidelines suggest a moderate protein diet - about 0.8 grams per kilogram of body weight per day. That’s roughly 50-60 grams for most adults. Too much protein forces your kidneys to work harder. Too little can cause muscle loss.
Don’t go on a high-protein keto diet. Don’t chug protein shakes. Stick to lean meats, eggs, dairy, beans, and tofu in reasonable portions. Talk to a dietitian who understands kidney health. They can help you balance nutrition without overloading your kidneys.
Remember: medication reduces protein leakage. Diet reduces the workload. Together, they’re powerful.
What’s Next?
Diabetic nephropathy is no longer a death sentence. With the right drugs, at the right doses, and the right lifestyle, you can keep your kidneys working for decades. The tools are here: ACE inhibitors, ARBs, SGLT2 inhibitors, and careful protein management.
But it’s not enough to have them. You have to use them correctly. Maximize the dose. Avoid dangerous combos. Watch for side effects. And never stop because of a small creatinine rise. That’s not failure - it’s proof the medicine is working.
Your kidneys are silent organs. They don’t hurt until it’s too late. Don’t wait for symptoms. Get your urine tested. Talk to your doctor about your meds. Take control - before your kidneys do.