Cumulative Drug Toxicity Calculator
Track Your Medication Exposure
See how much of high-risk medications you've accumulated over time. Based on medical guidelines for drugs with known cumulative toxicity risks.
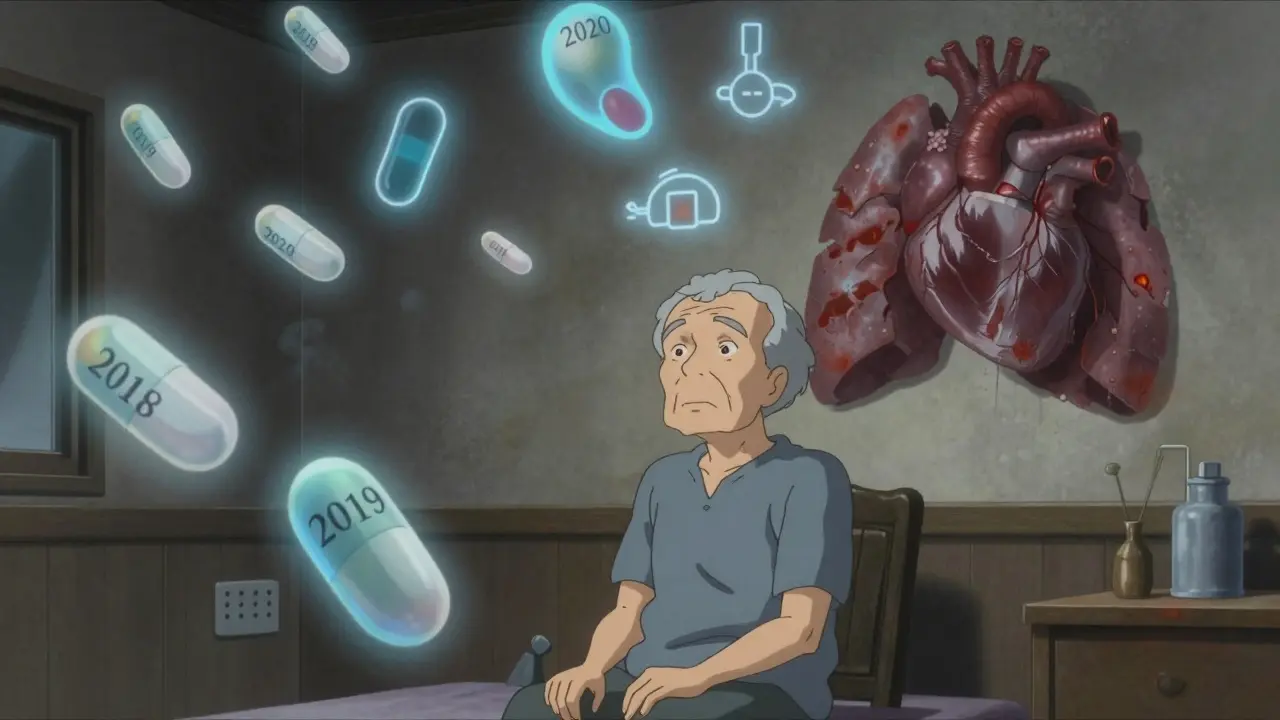
Most people think side effects show up right away-maybe a headache after taking a new pill, or nausea after the first dose of antibiotics. But what if the real danger isn’t in the first week? What if it’s in the fifth year?
That’s the quiet, dangerous truth about cumulative drug toxicity. It’s not the drug that hits you hard the first time. It’s the drug that sneaks in, stays, and slowly piles up-until your body can’t handle it anymore. And by then, it’s often too late to undo the damage.
How Your Body Can’t Keep Up
Your liver and kidneys are your body’s cleanup crew. They break down drugs and flush them out. But if you take a medication every day for months or years, and your body can’t clear it fast enough, it starts to stick around. This isn’t rare. It’s common.
Drugs with long half-lives-meaning they stay in your system for more than 24 hours-are the biggest culprits. Think amiodarone for heart rhythm, lithium for bipolar disorder, or digoxin for heart failure. These aren’t one-time fixes. They’re lifelong meds. And over time, even small daily doses add up. A study in the Journal of the National Cancer Institute found that after six cycles of cancer treatment, the chance of serious side effects jumped from under 25% to over 50%. That’s not a fluke. That’s math.
It gets worse if your liver or kidneys aren’t working perfectly. In older adults or people with chronic disease, these organs can lose 30-50% of their ability to process drugs. So what was a safe dose at 45 becomes dangerous by 65. And many patients never realize it-until they’re in the hospital with lung damage from amiodarone, or nerve pain from years of chemotherapy.
It’s Not Just Prescription Drugs
Cumulative toxicity isn’t limited to pills you get from a pharmacy. Fat-soluble vitamins like A, D, E, and K can build up too. Take too much vitamin D for years? You can develop calcium deposits in your blood vessels. Too much vitamin A? That can lead to liver scarring.
Heavy metals are another silent threat. Lead from old paint, mercury from certain fish, arsenic from contaminated water-these don’t vanish after one exposure. They settle into bones and fat, and over decades, they leak back into your bloodstream. That’s why some people develop unexplained fatigue, memory issues, or nerve damage decades after exposure.
Even some herbal supplements and over-the-counter painkillers play a role. Long-term use of NSAIDs like ibuprofen can quietly damage your kidneys. Acetaminophen, taken daily for arthritis, can slowly overwhelm the liver. These aren’t emergencies. They’re slow burns.
Why Doctors Miss It
Here’s the hard part: most doctors don’t track cumulative doses. They look at your last lab result, your last blood pressure reading. They don’t add up every pill you’ve taken since 2018.
One oncologist on Reddit shared a case: a patient on amiodarone had normal blood levels every checkup. But after taking 600 grams total over five years, she developed severe lung scarring. The drug was never above the "safe" level at any single point. But the total? Way over.
That’s the trap. Standard monitoring checks levels at a moment in time. Cumulative toxicity is about the sum of all moments. And unless someone is actively tracking the total dose, it’s invisible.
The American Geriatrics Society Beers Criteria lists 34 medications with high cumulative risk for older adults. For example, anthracycline chemotherapy drugs have a hard limit: 450 mg/m² total lifetime dose. Exceed that, and your heart is at serious risk. That number? Based on 8,500 patients across 17 clinical trials. But how many patients know their own cumulative limit? Very few.
Who’s Most at Risk?
It’s not just the elderly. It’s anyone on long-term meds:
- People taking anticoagulants like warfarin for atrial fibrillation
- Patients on methotrexate for rheumatoid arthritis or psoriasis
- Those on long-term antibiotics for acne or chronic infections
- People on psychiatric meds like lithium or valproate for years
- Anyone taking multiple drugs that are processed by the same liver enzyme
And it’s not just the drugs themselves. Environmental toxins-pesticides, air pollution, even some cosmetics-add to the burden. Ayurvedic medicine calls this "Dushi Visha," or chronic toxins. Modern science calls it cumulative toxicity. Same thing.
Medicare data shows 68% of adverse drug reactions in seniors are tied to long-term buildup-not new prescriptions. That’s not an accident. It’s a system failure.
What You Can Do
You can’t control everything. But you can control your awareness.
- Ask for your cumulative dose. If you’re on a drug for more than a year, ask your doctor: "What’s my total lifetime dose? Is there a safety limit?" Write it down.
- Know your meds. Keep a list of everything you take-prescription, OTC, supplements. Include dosage and how long you’ve been taking it.
- Get regular organ checks. If you’re on long-term meds, ask for annual liver and kidney function tests-even if you feel fine.
- Don’t assume "normal" labs mean safe. A normal level today doesn’t mean you haven’t built up too much over time.
- Talk to your pharmacist. Pharmacists are trained to track drug interactions and cumulative exposure. They’re your best ally.
A 2021 study in the Journal of Clinical Pharmacy and Therapeutics showed that when a rheumatology clinic started tracking methotrexate doses over time, serious side effects dropped by 37%. That’s not magic. That’s simple record-keeping.

The Bigger Picture
The global market for therapeutic drug monitoring is set to hit $4.7 billion by 2028. Why? Because hospitals and drug companies are finally waking up. The FDA now requires cumulative toxicity warnings on 78% of new cancer drugs. The European Medicines Agency made it mandatory for all chronic-use drugs starting in 2024.
But that’s the system. What about you?
Right now, only 38% of electronic health records can automatically track your total drug exposure. Most still rely on paper charts, memory, or guesswork. That’s dangerous.
Imagine if your phone could track your steps. Why shouldn’t your health record track your drug exposure?
It’s time to stop treating medications like they’re harmless. Even the safest drugs can turn toxic if you take them long enough. The body doesn’t forget. It remembers every dose. And sometimes, it pays the price years later.
You don’t need to stop your meds. But you do need to know how much you’ve taken. And why it matters.
Can cumulative drug toxicity be reversed?
Sometimes, yes-but not always. If caught early, stopping the drug and supporting liver or kidney function can help the body clear the buildup. But damage like lung fibrosis from amiodarone or heart muscle scarring from chemotherapy may be permanent. Early detection is key.
Which medications are most likely to cause cumulative toxicity?
Common ones include amiodarone (heart), lithium (bipolar), digoxin (heart), methotrexate (autoimmune), aminoglycoside antibiotics (infections), and anthracycline chemotherapy drugs. Fat-soluble vitamins (A, D, E, K) and heavy metals like lead or mercury also accumulate over time.
Do over-the-counter drugs cause cumulative toxicity?
Yes. Long-term daily use of NSAIDs like ibuprofen or naproxen can damage kidneys. Daily acetaminophen can stress the liver. Even high-dose vitamin D supplements over years can lead to calcium buildup in arteries. Just because it’s sold without a prescription doesn’t mean it’s safe for lifelong use.
Why don’t doctors always track cumulative doses?
Most electronic health records don’t calculate total lifetime exposure. Doctors focus on current symptoms and recent labs. Tracking cumulative doses takes time, manual effort, and often isn’t built into standard care. Many providers simply don’t know the limits for their patients’ meds.
How can I find out my own cumulative drug exposure?
Start by gathering your medication history: name, dose, start date, and duration. Ask your pharmacist to help calculate total exposure for high-risk drugs like amiodarone or methotrexate. Request copies of past lab reports to see if organ function has changed over time. If you’re on a long-term medication, ask your doctor: "Is there a maximum lifetime dose? How close am I to it?"
What to Do Next
If you’ve been on the same medication for more than three years, don’t wait for symptoms. Take action now.
- Make a list of every drug you’ve taken in the last five years.
- Call your pharmacy-they can print out your full dispensing history.
- Schedule a visit with your doctor or pharmacist to review cumulative risks.
- Ask for a liver and kidney function test if you haven’t had one in the past year.
Cumulative toxicity doesn’t announce itself with a siren. It whispers. And by the time you hear it, it’s often too late. Be the person who listens early.






