Medication Risk Assessment for Heart Rhythm Problems
Check Your Medication Risks
Identify if your medications could be contributing to heart rhythm problems. Over 400 common drugs can cause dangerous heart rhythm issues.
More than 400 common medications can trigger dangerous heart rhythm problems - and most people have no idea. It’s not just about heart pills. Your allergy medicine, antibiotic, antidepressant, or even your diabetes drug could be quietly messing with your heartbeat. These aren’t rare side effects. They’re real, preventable, and often missed until it’s too late.
What Exactly Is a Drug-Induced Arrhythmia?
A drug-induced arrhythmia happens when a medication interferes with the electrical signals that keep your heart beating regularly. This isn’t just a flutter. It can mean your heart skips, races, or goes into a dangerous rhythm like torsades de pointes - a type of ventricular arrhythmia that can lead to sudden cardiac arrest.
The most common way this happens is through QT interval prolongation. The QT interval is the time your heart takes to recharge between beats. When it’s too long, your heart becomes electrically unstable. Over 25 medications now carry FDA black box warnings for this exact risk. That’s the strongest warning the agency gives.
It’s not just about one drug. The risk jumps 300 to 500% when you take two or more QT-prolonging drugs together. That’s why someone on an antibiotic for a sinus infection, plus an antihistamine for allergies, and a statin for cholesterol might suddenly feel off - even if none of those drugs are meant to affect the heart.
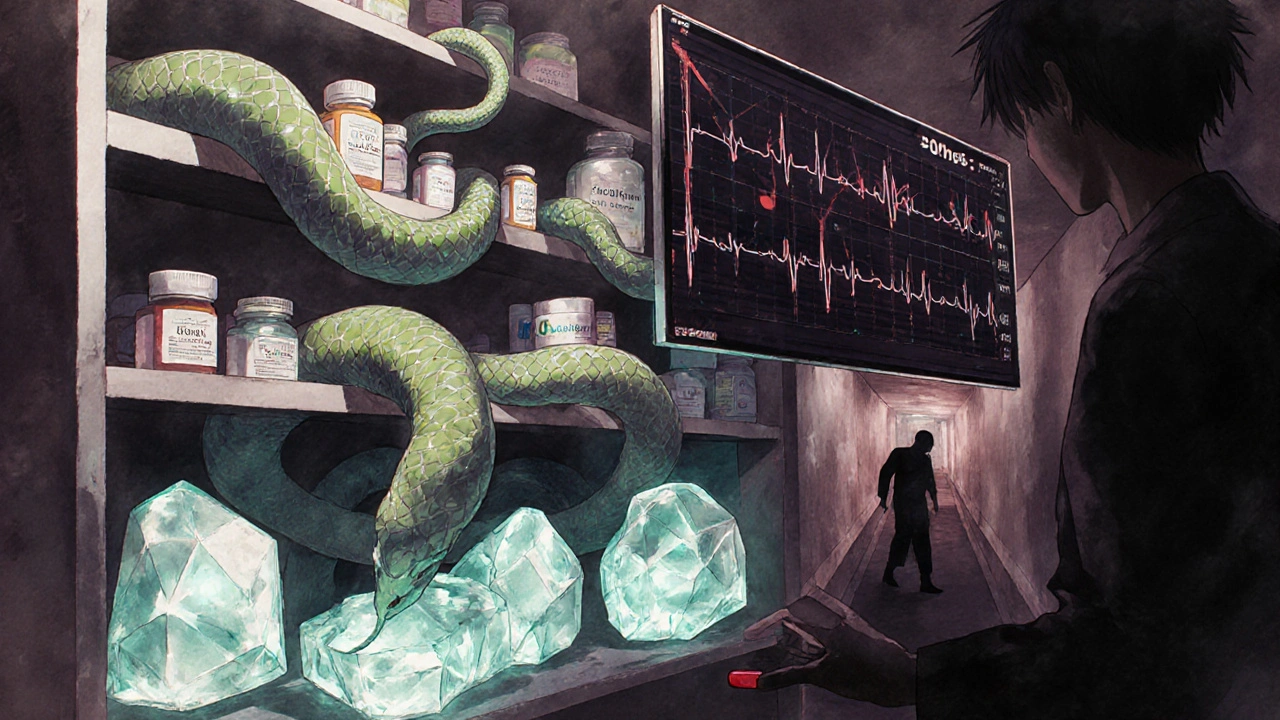
Which Medications Are Most Likely to Cause Problems?
Some of the most surprising culprits aren’t heart drugs at all. Here’s what to watch for:
- Antibiotics: Azithromycin and moxifloxacin can prolong QT in 3-5% of users, especially in the first week. This isn’t theoretical - emergency rooms see this every month.
- Antidepressants and antipsychotics: Citalopram, escitalopram, quetiapine, and risperidone are linked to arrhythmias. Even at standard doses, they can be risky for older adults or those with existing heart conditions.
- Anti-nausea drugs: Ondansetron (Zofran) and metoclopramide are common after surgery or chemo, but they carry a known risk of sudden arrhythmias.
- Diuretics: Furosemide and hydrochlorothiazide drain potassium and magnesium. Low levels of these minerals make your heart extra sensitive to any drug that affects its rhythm.
- Even heart rhythm drugs: Flecainide, propafenone, and amiodarone can cause the very arrhythmias they’re meant to treat. Amiodarone, for example, can trigger atrial fibrillation in 2-5% of patients due to thyroid effects.
- Beta-blockers: While they slow the heart for good reason, too much can cause dangerous bradycardia - heart rates below 50 bpm - leading to dizziness, fainting, or fatigue in 15-20% of users.
- Digoxin: Used for heart failure and atrial fibrillation, it becomes toxic when kidney function drops or magnesium levels fall. Toxicity can cause fast, irregular beats with heart block - a deadly combo.
And here’s something few doctors mention: Your genes matter. About 15% of people of African ancestry carry the S1103Y variant, and 12% of East Asians carry R1193Q. These variants make your heart cells far more likely to go haywire when exposed to QT-prolonging drugs. Genetic testing isn’t routine - but it should be considered if you’ve had unexplained arrhythmias or family history of sudden cardiac death.

Warning Signs You Can’t Ignore
These symptoms aren’t "just stress" or "getting older." If you’re on any medication and notice one or more of these, act fast:
- Palpitations: A pounding, fluttering, or irregular heartbeat. Reported in 70-80% of cases.
- Dizziness or lightheadedness: Especially when standing up. This often means your heart isn’t pumping enough blood to your brain.
- Fatigue: Unexplained exhaustion, even after sleep. Not just tired - drained.
- Chest discomfort: Not always a classic heart attack pain. Could be pressure, tightness, or just a weird ache.
- Fainting or near-fainting: Syncope is a red flag. If you’ve passed out, even briefly, get checked immediately.
One patient I spoke with - a 68-year-old woman in Bristol - started taking azithromycin for a chest infection. Two days later, she felt dizzy walking to the bathroom. She thought it was dehydration. By the third day, she collapsed. Her ECG showed torsades de pointes. She survived - but only because her husband called 999 right away.
How Doctors Manage Drug-Induced Arrhythmias
Good news: Most cases are reversible if caught early. Here’s what actually works:
- Stop or switch the drug: In 75-85% of cases, simply stopping or changing the medication fixes the problem. Your doctor may swap an antibiotic like azithromycin for one that doesn’t affect the QT interval.
- Correct electrolytes: Potassium and magnesium are critical. Doctors aim for potassium above 4.0 mEq/L and magnesium above 2.0 mg/dL. If you’re on diuretics, you may need supplements - but only under supervision. Too much potassium can be just as dangerous.
- Monitor with ECG: Before starting high-risk drugs, get a baseline ECG. Repeat it within 72 hours. If your QT interval extends more than 60 milliseconds from baseline, the drug should be reconsidered.
- Adjust beta-blocker doses: If you’re on metoprolol and feel fatigued or dizzy, your heart rate might be too low. Dose reduction helps 60-70% of patients. In rare cases, a pacemaker may be needed to allow safe continued use.
- Consider ablation: If the arrhythmia persists after stopping the drug, catheter ablation fixes the problem in 5-10% of cases. Surgery is needed in less than 2%.
It’s not just about the drug. Lifestyle matters too. Smoking, heavy alcohol (more than 3 drinks a day), and poor sleep all raise your risk. Caffeine? It causes palpitations in 25-30% of people, but serious arrhythmias from caffeine alone are rare. Still, if you’re on a QT-prolonging drug, cutting back helps.
Why This Is So Common - And So Preventable
Drug-induced arrhythmias cause 100,000-150,000 hospitalizations in the U.S. every year. That’s more than many cancers. The cost? Over $1.2 billion annually.
Why does this keep happening? Because doctors don’t always think about drug interactions. Pharmacists don’t always flag them. Patients don’t know to report dizziness as a possible heart sign.
The good news? We’re getting better. The American College of Cardiology is launching a decision-support tool in 2024 that calculates your personal risk based on age, meds, kidney function, electrolytes, and genetic markers. It’s not everywhere yet - but it’s coming.
Meanwhile, you can protect yourself:
- Always tell your doctor all the medications you take - including OTC, supplements, and herbal products.
- Ask: "Could this drug affect my heart rhythm?" Especially if you’re over 65, have kidney disease, or take more than five meds.
- Keep a list of your meds and share it at every appointment.
- If you feel new dizziness, palpitations, or fatigue after starting a new drug - don’t wait. Call your doctor. Go to urgent care.
What You Should Do Right Now
If you’re on any of the medications listed above - or have any unexplained symptoms - here’s your action plan:
- Check your current medications against the list above.
- Review your last blood test. Are your potassium and magnesium levels normal?
- Ask your doctor if you’ve had a recent ECG. If not, request one.
- Write down any new symptoms - even if they seem minor. Note when they started and what you were taking.
- Don’t stop any medication without talking to your doctor. But do speak up.
Heart arrhythmias from meds are not a fluke. They’re a predictable, preventable problem. The tools to stop them exist. What’s missing is awareness. You don’t need to be a doctor to protect your heart. You just need to ask the right questions - and listen to your body.
Can over-the-counter drugs cause heart arrhythmias?
Yes. Common OTC drugs like antihistamines (diphenhydramine in Benadryl), decongestants (pseudoephedrine), and certain cough syrups (containing dextromethorphan) can prolong the QT interval. Even herbal supplements like licorice root or ephedra can trigger dangerous rhythms. Always check labels and ask a pharmacist if you’re on heart medication or have a history of arrhythmias.
Is it safe to take antibiotics if I have a history of heart rhythm problems?
It depends. Macrolides like azithromycin and fluoroquinolones like moxifloxacin carry higher risk. If you’ve had prior arrhythmias, your doctor should choose an alternative - like amoxicillin or doxycycline - that doesn’t affect the QT interval. Always disclose your full cardiac history before any antibiotic is prescribed.
How long does it take for a drug-induced arrhythmia to go away after stopping the medication?
In most cases, the rhythm normalizes within days to a week after stopping the drug - especially if electrolytes are corrected. But in rare cases, especially with amiodarone or long-term use, effects can linger for weeks or months. Follow-up ECGs are essential to confirm recovery.
Can stress or anxiety cause the same symptoms as a drug-induced arrhythmia?
Yes - but the difference matters. Anxiety can cause palpitations and dizziness, but it rarely causes prolonged QT or sustained dangerous rhythms like torsades. If you’re on a high-risk medication and feel these symptoms, don’t assume it’s anxiety. Get an ECG to rule out a drug effect. Your heart can’t tell the difference - but your doctor can.
Should I get genetic testing before taking a new medication?
Not routinely - yet. But if you’ve had unexplained fainting, a family history of sudden cardiac death, or survived a drug-induced arrhythmia, genetic testing for variants like S1103Y or R1193Q may be warranted. Some hospitals now offer pharmacogenetic screening before prescribing high-risk drugs. Ask your cardiologist or pharmacist if it’s available to you.