Every year, millions of people in the U.S. and UK take SSRIs to manage depression, anxiety, or OCD. These medications work by boosting serotonin - a brain chemical tied to mood - and for many, they’re life-changing. But here’s something most people don’t know: mixing SSRIs with even a common painkiller or herbal supplement can trigger a dangerous, sometimes deadly, reaction called serotonin syndrome.
What Is Serotonin Syndrome?
Serotonin syndrome isn’t just a side effect. It’s a medical emergency. It happens when too much serotonin builds up in your nervous system. This isn’t about feeling a little more anxious or sweaty - it’s about your body going into overdrive. Symptoms can show up within hours and include:- Shivering or uncontrollable muscle twitching
- Heavy sweating, even when it’s cool
- High fever (over 38°C or 100.4°F)
- Muscle stiffness or rigidity
- Rapid heartbeat, high blood pressure
- Confusion, agitation, or hallucinations
If you’re on an SSRI and start feeling this way after adding a new medication, supplement, or even changing your dose - get help immediately. Left untreated, serotonin syndrome can lead to seizures, kidney failure, or death.
Which Medications Are the Biggest Risk?
Not all drug combinations are equal. Some are barely risky. Others are ticking time bombs. Here’s what the data says:MAOIs are the worst. These older antidepressants - like phenelzine or selegiline - should never be taken with SSRIs. The FDA and UK drug regulators call this combination contraindicated for a reason. When mixed, serotonin levels spike dangerously fast. Studies show mortality rates between 30% and 50% in these cases.
Linezolid, an antibiotic used for tough infections, is another hidden danger. It blocks serotonin breakdown like an MAOI. A 2022 JAMA study found people over 65 on SSRIs who took linezolid were nearly three times more likely to develop serotonin syndrome. Even a 5-day course can be enough.
Tramadol, dextromethorphan, and pethidine - common painkillers and cough syrups - are high-risk too. Tramadol, in particular, is often prescribed for back pain or arthritis. But when paired with sertraline or fluoxetine, it can push serotonin levels over the edge. One Reddit user described hospitalization after taking tramadol with sertraline: “My legs wouldn’t stop moving. My temperature hit 104.2°F.”
Meanwhile, codeine, morphine, and oxycodone show little to no increased risk. If you need pain relief while on an SSRI, these are safer choices.
What About Over-the-Counter and Herbal Products?
You might not think of St. John’s wort as a drug - but it’s a powerful serotonin booster. People take it for “natural” mood support, not realizing it’s chemically similar to SSRIs. A user on Drugs.com reported confusion and violent shivering after combining it with Prozac for just three days. The ER doctor diagnosed early serotonin syndrome.Other risky supplements include tryptophan, 5-HTP, and even some energy drinks with high doses of L-tryptophan. Even melatonin, often used for sleep, can add up in combination with SSRIs - especially in older adults taking multiple meds.
And don’t forget triptans, the migraine drugs like sumatriptan. They’re not antidepressants, but they act on serotonin receptors. The FDA added a black box warning in 2006 about combining them with SSRIs or SNRIs. Many doctors still miss this interaction.
Why Are Some SSRIs Riskier Than Others?
Not all SSRIs are created equal. Their chemical makeup affects how long they stay in your body and how strongly they block serotonin reuptake.- Paroxetine has the strongest serotonin reuptake inhibition - up to 95% - making it the most likely to cause problems in combinations.
- Fluoxetine sticks around for weeks. Even after you stop taking it, norfluoxetine (its active metabolite) can linger for up to 15 days. Switching to an MAOI? You need to wait five weeks, not two.
- Sertraline and escitalopram are shorter-acting and less potent, which is why they’re often first-line choices. But they’re still risky when mixed with other serotonergic drugs.
That’s why timing matters. If you’re switching from one antidepressant to another, your doctor needs to know the half-life of each. Rushing the transition is a leading cause of serotonin syndrome.
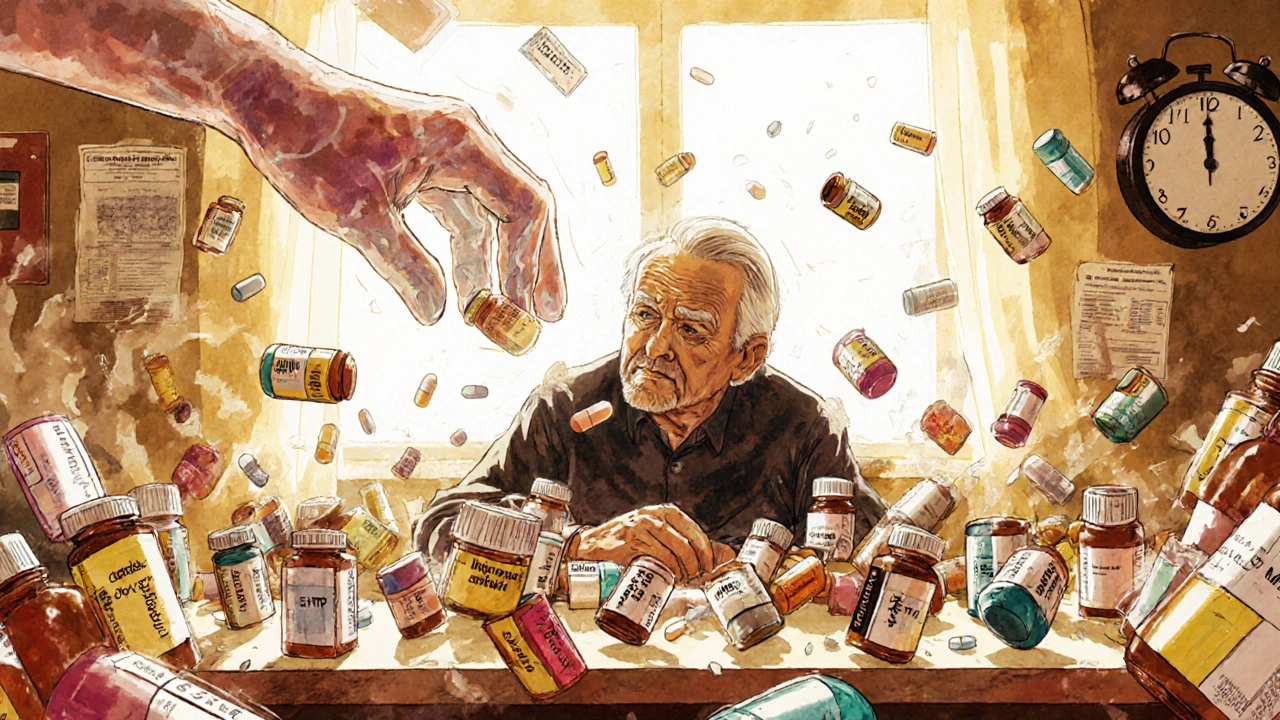
Who’s Most at Risk?
It’s not just about what you take - it’s how many things you take. The average American over 65 is on five or more medications. Many of them are prescribed by different doctors, with no one looking at the full picture.Studies show:
- 21.5% of Americans over 60 take an SSRI
- 18.3% take an opioid for chronic pain
- More than 22% of seniors take five or more drugs daily
That’s a perfect storm. Add in genetic factors - like being a poor metabolizer of CYP2D6 enzymes - and your risk doubles. This is why older adults are disproportionately affected. A 2023 FDA analysis found serotonin syndrome cases spiked in patients over 65 on SSRI-opioid combos.
How to Stay Safe
You don’t have to avoid SSRIs. But you do need to be smart.1. Tell every doctor - every time. Whether it’s your dentist, GP, or pain specialist, say: “I’m on an SSRI.” Don’t assume they’ll check your chart.
2. Ask your pharmacist. Pharmacists are trained to catch dangerous combinations. A 2023 study found pharmacist-led reviews reduced serotonin syndrome events by 47% in Medicare patients.
3. Know the 5 S’s. The Cleveland Clinic recommends watching for:
- Shivering
- Sweating
- Stiffness
- Seizures (rare, but serious)
- Sudden confusion
If two or more appear after starting a new drug - go to the ER. Don’t wait.
4. Avoid high-risk combos entirely. Never mix SSRIs with MAOIs, linezolid, or methylene blue. If you need an antibiotic, ask for one that doesn’t affect serotonin.
5. Use opioid painkillers wisely. Choose morphine or oxycodone over tramadol, dextromethorphan, or pethidine. The CDC now explicitly recommends this in its 2024 opioid prescribing guidelines.
What’s Changing?
The system is catching up. In 2024, the FDA mandated that all electronic prescribing systems must now show automatic alerts when a doctor tries to prescribe an SSRI with a high-risk drug. Hospitals using Epic Systems saw a 32% drop in dangerous SSRI-opioid combos after this update.There’s also promising research. A new blood test called SerotoninQuant is in phase 3 trials at Mayo Clinic. By 2026, it might give doctors an objective way to diagnose serotonin syndrome - instead of relying on symptoms that look like the flu, heatstroke, or a panic attack.
Bottom Line
SSRIs are safe - when used correctly. But they’re not harmless. The biggest danger isn’t the pill itself. It’s the other pills, supplements, and painkillers stacked on top of it. Thousands of cases are preventable. You just need to know the risks, speak up, and ask questions.If you’re on an SSRI and your doctor wants to add something new - pause. Ask: “Could this raise my serotonin levels?” If they don’t know, ask for a pharmacist to review your full list. Your life might depend on it.
Can serotonin syndrome happen with just one SSRI?
Rarely. Serotonin syndrome almost always happens when SSRIs are combined with another serotonergic drug - like an opioid, another antidepressant, or an herbal supplement. Taking an SSRI alone at the right dose is very unlikely to cause it. The risk jumps dramatically with combinations.
How long after starting a new drug does serotonin syndrome appear?
Symptoms usually start within hours - often within 2 to 6 hours after taking the new medication. In some cases, they can appear up to 24 hours later. If you’ve just added tramadol, St. John’s wort, or a new painkiller to your SSRI, watch closely during this window.
Is serotonin syndrome the same as an SSRI overdose?
No. An overdose means you took too much of one drug - like swallowing 20 pills. Serotonin syndrome is about drug interactions - even normal doses of two different drugs can cause it. You can have serotonin syndrome without taking too much of anything.
Can I take ibuprofen or acetaminophen with an SSRI?
Yes. Ibuprofen and acetaminophen (Tylenol) do not affect serotonin levels and are safe to use with SSRIs. They’re preferred over opioids like tramadol or codeine if you need pain relief.
What should I do if I think I have serotonin syndrome?
Go to the emergency room immediately. Do not wait. Tell them you’re on an SSRI and recently started a new medication. Early treatment - stopping the trigger drugs and giving supportive care - can save your life. Delaying care increases the risk of organ failure or death.
Are there any safe antidepressants to take with SSRIs?
Generally, no. Combining SSRIs with other antidepressants (like SNRIs, trazodone, or mirtazapine) increases serotonin syndrome risk by over three times. If your SSRI isn’t working, your doctor should adjust the dose or switch you entirely - not add another antidepressant. There are safer alternatives, like therapy or lifestyle changes, that can be tried first.