When you’re stuck in a fog that won’t lift-no matter how hard you try to shake it-you’re not weak. You’re not lazy. You might be dealing with major depressive disorder (MDD). It’s not just feeling sad. It’s losing interest in everything you once loved. It’s waking up exhausted, even after eight hours of sleep. It’s feeling like a burden, even when people tell you you’re not. And it’s more common than you think: about 1 in 6 U.S. adults experience it in a given year, according to NAMI’s 2025 data.
The good news? You don’t have to live like this forever. Treatment works. And it doesn’t mean just popping pills or sitting in a therapist’s office once a month. There are real, science-backed options-and the right mix for you might be simpler than you imagine.
What Exactly Is Major Depressive Disorder?
MDD isn’t a phase. It’s not something you can ‘snap out of.’ It’s a medical condition with real biological underpinnings. Symptoms last at least two weeks and include:
- Constant low mood or irritability
- Loss of pleasure in hobbies, food, sex, or socializing
- Changes in sleep-too much or too little
- Weight loss or gain without trying
- Feeling worthless or guilty for no reason
- Trouble focusing, making decisions, or remembering things
- Thoughts of death or suicide
It can show up after a breakup, job loss, or illness. Or it can just show up-with no obvious trigger. That’s part of what makes it so confusing. You might think, ‘I have everything to be happy about,’ but your brain isn’t responding the way it used to. That’s not your fault.
Psychotherapy: Talking Your Way Out of the Dark
Therapy isn’t just ‘talking.’ It’s learning new ways to think, feel, and act. The most effective types for MDD are backed by decades of research.
Cognitive Behavioral Therapy (CBT) is the gold standard. It helps you spot thoughts like ‘I’m a failure’ or ‘Nothing will ever get better’ and test them against reality. Instead of believing those thoughts, you learn to ask: ‘Is this true? What’s the evidence?’ A 2021 study in PMC showed CBT reduces depressive symptoms by rewiring how the brain processes negative information. It’s not magic-it’s practice. You’ll get homework: journaling, tracking moods, challenging distorted beliefs. It takes time-usually 12 to 20 sessions-but the skills stick. One Reddit user said, ‘CBT taught me skills I still use five years later.’
Behavioral Activation is CBT’s simpler cousin. It doesn’t focus on thoughts. It focuses on action. When you’re depressed, you stop doing things. You cancel plans. You stay in bed. This makes depression worse. Behavioral activation says: ‘Do one small thing that used to give you a spark-even if you don’t feel like it.’ Walk around the block. Call a friend. Water a plant. Do it even if you feel nothing. Over time, doing things rebuilds your sense of control and connection.
Interpersonal Therapy (IPT) looks at your relationships. Depression often grows in the soil of loneliness, conflict, or grief. IPT helps you navigate breakups, family tension, or job loss by improving communication and setting boundaries. It’s especially helpful if your mood dips every time you argue with your partner or feel isolated after a loss.
And yes, therapy can be digital. Computerized CBT (CCBT) platforms like SilverCloud or MoodGYM offer structured online programs. They’re great if you live in a rural area, have mobility issues, or can’t find a therapist nearby. But they’re not for everyone. You need to be motivated. No therapist is there to nudge you if you skip a session.
Antidepressants: How They Work and What to Expect
If therapy feels too slow-or your symptoms are severe-medication can help. Antidepressants don’t make you ‘happy.’ They help your brain get back to baseline. Think of them like insulin for diabetes: they correct a chemical imbalance, not create something new.
SSRIs (Selective Serotonin Reuptake Inhibitors) are usually the first choice. They include escitalopram (Lexapro), sertraline (Zoloft), and fluoxetine (Prozac). They’re safe, well-studied, and have fewer side effects than older drugs. But they don’t work overnight. Most people feel a little better after 2-4 weeks. Full effect takes 8-12 weeks. And yes-some feel worse before they feel better. Nausea, headaches, and emotional numbness are common early side effects. One user on HealthUnlocked wrote: ‘I waited 8 weeks for Prozac to work and felt worse before better.’
SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors) like venlafaxine (Effexor) and duloxetine (Cymbalta) work on two neurotransmitters. They’re often used when SSRIs don’t help or if you have chronic pain along with depression.
Mirtazapine and amitriptyline are older but still effective. Mirtazapine can help with sleep and appetite loss. Amitriptyline works well but has more side effects-dry mouth, dizziness, weight gain-so it’s usually a second-line option.
Not all antidepressants work for everyone. That’s normal. If one doesn’t help after 6-8 weeks, your doctor might switch you. It’s not failure. It’s trial and error. And yes, side effects like weight gain or sexual dysfunction happen. But they often improve over time-or can be managed by changing the dose or medication.

Combination Therapy: Why Two Tools Are Better Than One
Here’s the clearest finding from recent research: combining antidepressants with CBT works better than either alone, especially for moderate to severe depression. A 2025 study in Nature confirmed this. The medication helps you feel well enough to engage in therapy. The therapy helps you stay well after you stop the medication.
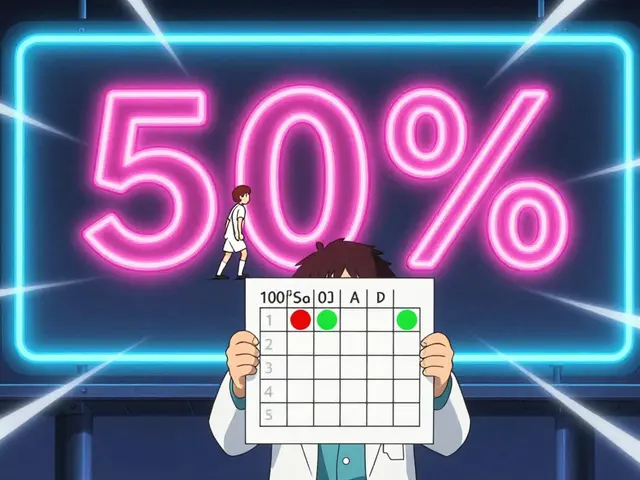
Medication alone? It reduces symptoms. But relapse rates are high-up to 50% within a year after stopping. Therapy alone? It’s just as effective as meds for mild to moderate cases. But it builds tools that last. You learn to recognize early warning signs. You know how to handle stress without falling back into the dark.
For severe depression (PHQ-9 score ≥16), NICE guidelines strongly recommend both. If you’re having thoughts of suicide or can’t get out of bed, starting medication early can be life-saving. Then, therapy helps you rebuild.
What About Other Treatments?
When meds and therapy don’t work, options still exist.
Electroconvulsive Therapy (ECT) sounds scary, but it’s one of the most effective treatments for treatment-resistant depression. It’s done under anesthesia. A small electric current triggers a brief seizure. It resets brain activity. Many patients report dramatic improvement within days. Side effects? Temporary memory gaps. But for those who’ve tried everything else, it’s often the only thing that works.
Transcranial Magnetic Stimulation (TMS) is non-invasive. It uses magnetic pulses to stimulate areas of the brain linked to mood. It’s FDA-approved, covered by many insurers, and has few side effects. You go in for 20-40 minutes, 5 days a week, for 4-6 weeks. No anesthesia. No recovery time.
And yes-some people try supplements like omega-3s or St. John’s Wort. But don’t rely on them. They’re not proven for MDD. And they can interfere with antidepressants. Always talk to your doctor before trying anything new.

Access, Cost, and Real-Life Barriers
Knowing what works is one thing. Getting it is another.
Waiting lists for NHS talking therapies in the UK can stretch for months. In rural areas, therapists are scarce. Telehealth helps-but only if you have reliable internet. And therapy costs? In the U.S., $100-$200 per session. Even with insurance, copays add up.
Medication costs vary. Generic SSRIs like sertraline can be as cheap as $4 a month. Others cost more. If you’re struggling to pay, ask your doctor about patient assistance programs. Many drugmakers offer them.
And stigma? Still real. Some people think therapy is ‘for crazy people.’ Or that taking antidepressants means you’re ‘weak.’ But you wouldn’t tell someone with diabetes to stop using insulin. Depression is a medical condition. Treating it isn’t surrender. It’s self-care.
How to Start
Step one: Talk to your GP. They can screen you with a simple questionnaire (like the PHQ-9). They can refer you to local therapy services or prescribe medication.
Step two: Ask questions. What are my options? What are the side effects? How long until I feel better? What if it doesn’t work? Don’t be afraid to push for answers.
Step three: Try one thing. Don’t try everything at once. Start with therapy or medication-not both. See what fits. You can always add the other later.
Step four: Be patient. Healing isn’t linear. Some days will be better. Some will feel like the first day. That’s normal. Progress isn’t always obvious. But it’s happening.
You don’t have to do this alone. The NAMI HelpLine is open 24/7 at 988. Text ‘NAMI’ to 62640. Call 800-950-6264. They’ve heard it all. They won’t judge. They’ll help you find the next step.
What’s Next?
Science is moving fast. Researchers are testing genetic tests to predict which antidepressant will work best for you. Apps are being developed to track mood and send alerts when you’re slipping. Digital CBT is becoming standard in the NHS.
But the core hasn’t changed: depression is treatable. You’re not broken. You’re not alone. And you don’t have to wait until you’re at rock bottom to get help. Start now. One step. One day. One therapy session. One pill. It adds up.
Can antidepressants make me feel emotionally numb?
Yes, some people report feeling emotionally flat or detached when taking SSRIs or SNRIs. This isn’t universal, but it’s common enough that doctors know to watch for it. If you feel this way, don’t stop the medication abruptly. Talk to your doctor. Sometimes lowering the dose helps. Other times, switching to a different medication-like mirtazapine or bupropion-can reduce emotional blunting while still treating depression.
How long should I stay on antidepressants?
Most doctors recommend staying on antidepressants for at least 6 to 12 months after symptoms improve. For people with recurrent depression or severe episodes, longer-term use (2+ years) may be advised. Stopping too soon increases the risk of relapse. Never stop cold turkey-withdrawal can cause dizziness, nausea, or mood swings. Always taper off under medical supervision.
Is therapy better than medication for depression?
For mild to moderate depression, therapy (especially CBT) is just as effective as medication. For severe depression, combining both is more effective than either alone. Therapy teaches coping skills that last after treatment ends. Medication can provide faster relief when symptoms are overwhelming. The best choice depends on your symptoms, history, preferences, and access to care.
Can I do CBT on my own without a therapist?
Yes, but with caveats. Computerized CBT (CCBT) programs like Beating the Blues or MoodGYM are evidence-based and can help. They’re great for mild depression or as a supplement. But if you’re severely depressed, struggling to focus, or feel hopeless, working with a trained therapist is far more effective. A therapist adapts to your needs, corrects misunderstandings, and builds a supportive relationship-something apps can’t replicate.
What if I don’t believe in therapy or medication?
It’s okay to be skeptical. Many people are. But depression isn’t a matter of belief-it’s a medical condition. If you’re unsure, try one small step: a 10-minute chat with your doctor, or a free online CBT module. You don’t have to commit to years of therapy or lifelong pills. Start small. See what happens. You might be surprised. And if it doesn’t work for you, that’s fine too. There are other options-like exercise, light therapy, or TMS-that might fit better.