Menopause Symptom Tracker
Track Your Symptoms
Select symptoms you're experiencing. This tool estimates your severity score based on national study data.
Your Symptom Score
0 out of 10
When you hear the word Menopause is the permanent end of menstrual cycles, typically occurring between ages 45 and 55, caused by a sharp decline in ovarian hormone production, a lot of images pop into mind-sweaty nights, sudden mood swings, and a sudden loss of femininity. Those pictures are half‑truth, half‑exaggeration. In this article we’ll separate the hype from the health facts, show you the truly common symptoms, and give you practical ways to tell myth from reality.
Quick Takeaways
- Hot flashes and night sweats affect about 75% of women, but they usually lessen after two years.
- Sleep disruption, mood changes, and vaginal dryness are real, hormone-driven symptoms.
- Weight gain, severe depression, and sudden memory loss are not caused by menopause alone; other health factors are often at play.
- Bone loss and heart‑health risks rise after menopause because of lower Estrogen levels, not because the transition itself is “dangerous.”
- Lifestyle tweaks-regular exercise, balanced diet, and stress management-cut symptom severity for most women.
Myth #1: Menopause Is a Sudden Event That Happens Overnight
Many pop‑culture references describe menopause as a single, dramatic switch‑off. In reality, menopause is the final stage of a gradual process called Perimenopause. During perimenopause, hormone levels swing wildly, causing irregular cycles and early symptoms. The official definition of menopause is confirmed only after 12 consecutive months without a period.
Myth #2: Only Hot Flashes Define Menopause
Hot flashes-sudden waves of heat that can last from a few seconds to several minutes-are the most publicized symptom, but they only tell part of the story. According to a 2023 study from the North American Menopause Society, about 75% of women report hot flashes, yet roughly 30% never experience them at all. Let’s look at the broader symptom list.
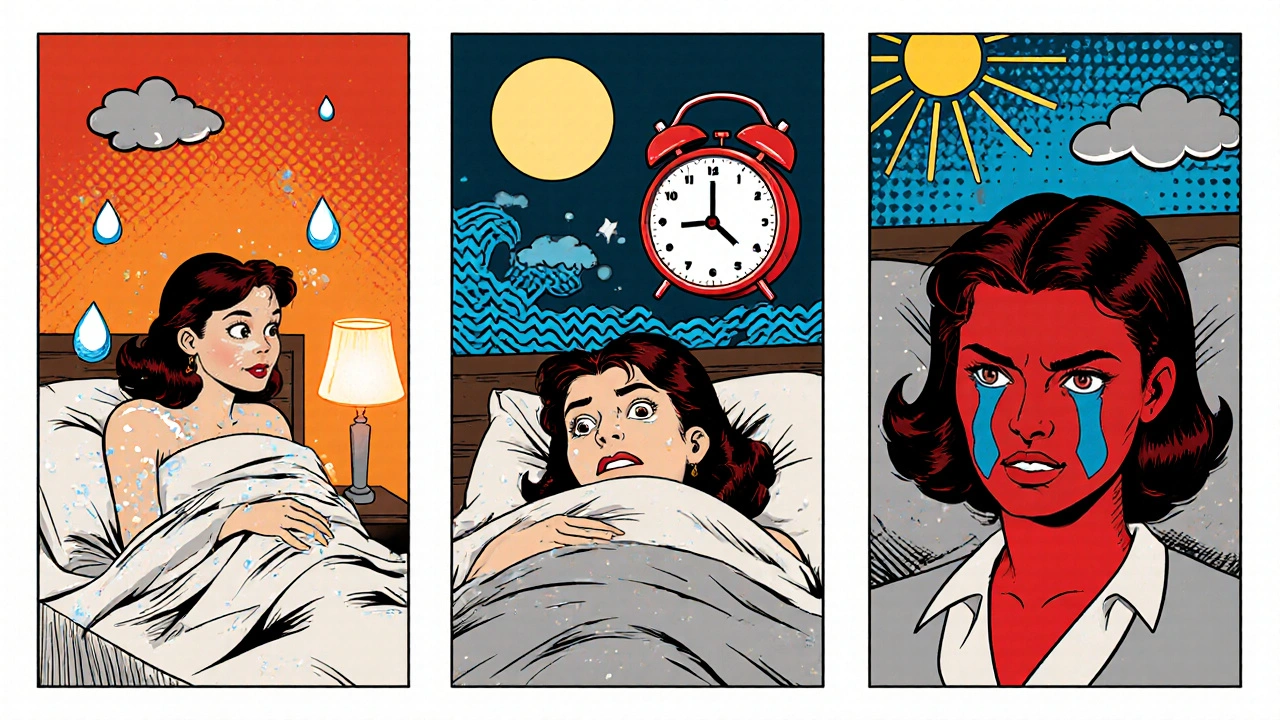
Real Symptom #1: Night Sweats
Night sweats are essentially hot flashes that strike while you’re in bed. They can disrupt sleep, lead to fatigue, and cause clothing changes. The same 2023 study found that 60% of women who have hot flashes also report night sweats, making them the second most common symptom.
Real Symptom #2: Sleep Disturbances
Beyond night sweats, many women struggle with difficulty falling asleep or staying asleep. Hormonal shifts affect the body’s internal clock, and the anxiety about triggering a hot flash can create a feedback loop. A 2024 sleep‑medicine review notes that 45% of menopausal women experience insomnia at some point.
Real Symptom #3: Mood Swings & Irritability
Fluctuating Estrogen levels influence neurotransmitters like serotonin and dopamine. This can make emotions feel amplified-short temper, tearfulness, or a sense of “on‑edge” is common. Importantly, severe depression is not a direct result of menopause; it often signals an underlying mood disorder that should be evaluated by a professional.
Real Symptom #4: Vaginal Dryness & Discomfort
As estrogen drops, the vaginal lining thins, losing its natural lubrication. This can cause itching, burning, or painful intercourse (dyspareunia). Over‑the‑counter moisturizers and prescription low‑dose estrogen gels can restore comfort.
Real Symptom #5: Bone Density Loss (Osteoporosis)
Estrogen protects bone by slowing the activity of cells that break down bone tissue. After menopause, bone loss accelerates, increasing fracture risk. The International Osteoporosis Foundation estimates that women lose up to 2% of bone density per year for the first five years post‑menopause. Calcium, vitaminD, weight‑bearing exercise, and sometimes bisphosphonate meds help mitigate the decline.
Real Symptom #6: Heart‑Health Changes
Cardiovascular disease becomes the leading cause of death for women after menopause, largely because estrogen’s favorable effect on cholesterol and blood vessels wanes. A 2022 meta‑analysis showed that post‑menopausal women have a 20% higher risk of heart attack compared with pre‑menopausal peers. Lifestyle measures-regular aerobic activity, a Mediterranean‑style diet, and blood‑pressure monitoring-are crucial.
Myth #3: Menopause Guarantees Weight Gain
Weight gain often coincides with menopause, but it’s not caused by the hormonal shift alone. Reduced muscle mass, slower metabolism, and lifestyle changes (lower activity, higher calorie intake) play larger roles. Resistance training can preserve muscle and keep metabolism humming.
Myth #4: Menopause Causes Memory Loss or “Brain Fog”
Many women report fleeting moments of forgetfulness, but research shows no permanent cognitive decline directly linked to menopause. A 2021 longitudinal study found that most “brain fog” resolves within a year and is more strongly associated with sleep loss and stress.

Myth #5: All Women Experience Severe Symptoms
Symptom severity varies widely. Genetics, ethnicity, smoking status, and overall health all influence the experience. For example, Japanese women report fewer and milder hot flashes than Western women, likely due to diet and lifestyle differences.
Practical Tips to Manage Real Symptoms
- Track Your Symptoms: Use a simple journal or an app to note hot flashes, sleep quality, and mood changes. Patterns help you and your clinician decide on treatment.
- Stay Cool: Dress in layers, keep your bedroom at 65‑68°F, and use breathable fabrics like cotton.
- Mind Your Diet: Incorporate phytoestrogen‑rich foods (soy, flaxseed), limit caffeine and alcohol, and aim for 5-7 servings of fruits/vegetables daily.
- Exercise Regularly: 150 minutes of moderate cardio plus two strength‑training sessions a week reduce hot flashes, improve mood, and protect bone.
- Stress Management: Yoga, mindfulness, or a hobby can lower cortisol, which otherwise may intensify hot flashes.
- Consider Hormone Therapy (HT): For many women, low‑dose estrogen combined with progesterone (if they have a uterus) eases a wide range of symptoms. Discuss risks-such as clotting or breast‑cancer history-with your doctor.
- Non‑Hormonal Options: SSRIs, gabapentin, and certain herbal extracts (black cohosh) have shown modest relief for hot flashes.
- Address Vaginal Health: Over‑the‑counter moisturizers, water‑based lubricants, or low‑dose vaginal estrogen are safe for most women.
Myth vs Fact Comparison
| Myth | Fact |
|---|---|
| Menopause happens overnight. | It follows a gradual transition called perimenopause; menopause is confirmed after 12 months without periods. |
| Only hot flashes are a symptom. | Night sweats, sleep issues, mood changes, vaginal dryness, bone loss, and heart‑health changes are also common. |
| All women gain significant weight. | Weight gain depends on diet, activity, and muscle loss; hormone changes alone are not the primary driver. |
| Memory loss is inevitable. | Short‑term “brain fog” can occur, often linked to sleep loss; permanent decline is not a direct result of menopause. |
| Hormone therapy is unsafe for everyone. | When properly prescribed, HT can safely relieve many symptoms; risks vary by individual health history. |
When to Seek Professional Help
If you notice any of the following, schedule a visit with a health‑care provider:
- Hot flashes that disrupt daily life despite lifestyle changes.
- Severe or prolonged sleep deprivation.
- Persistent low mood, anxiety, or thoughts of self‑harm.
- Vaginal pain that limits sexual activity.
- Signs of osteoporosis (fractures, loss of height) or heart‑health concerns (chest pain, shortness of breath).
Professional evaluation can rule out other conditions (thyroid disorders, anemia, depression) that mimic menopausal symptoms.
Bottom Line
Menopause is a natural life stage, not a disease. The most common real symptoms-hot flashes, night sweats, sleep disruption, mood swings, vaginal dryness, bone density loss, and heart‑health changes-are rooted in the drop of estrogen and progesterone. Myths about overnight onset, universal weight gain, and inevitable memory loss cloud the picture and can prevent women from seeking effective relief. By tracking symptoms, adopting healthy lifestyle habits, and consulting a clinician for personalized treatment, you can navigate menopause with confidence.
Frequently Asked Questions
How long do hot flashes usually last?
For most women, hot flashes peak during the first two years after menopause and gradually decrease. About 20% continue to experience them occasionally beyond ten years.
Can diet really reduce night sweats?
Yes. Cutting caffeine, alcohol, and spicy foods, while adding soy, flaxseed, and omega‑3‑rich fish, has been shown in several trials to lower the frequency of night sweats.
Is hormone therapy safe for heart health?
When started near the onset of menopause and used at the lowest effective dose, hormone therapy can actually improve cholesterol profiles and may lower heart‑attack risk for many women. Women with a history of clotting disorders or specific cancers should avoid it.
What non‑hormonal options help with hot flashes?
Low‑dose antidepressants (SSRIs/SNRIs), gabapentin, and some herbal supplements like black cohosh can provide modest relief. Acupuncture and paced breathing exercises are also reported to help some women.
How do I know if I’m losing bone density?
A dual‑energy X‑ray absorptiometry (DEXA) scan measures bone mineral density. Women should start screening at age 65, or earlier if they have risk factors like family history, smoking, or early menopause.