When you take your meds out of the original bottle and put them into a pillbox or a pharmacy-repackaged vial, you might think you’re just making life easier. But you’re also changing how that medicine behaves. The manufacturer’s expiration date? It no longer applies. That’s not a suggestion-it’s a fact backed by the FDA, USP, and every major pharmacy board in the U.S. And if you don’t know why, you’re risking your health-or someone else’s.
Why Original Expiration Dates Don’t Work for Repackaged Drugs
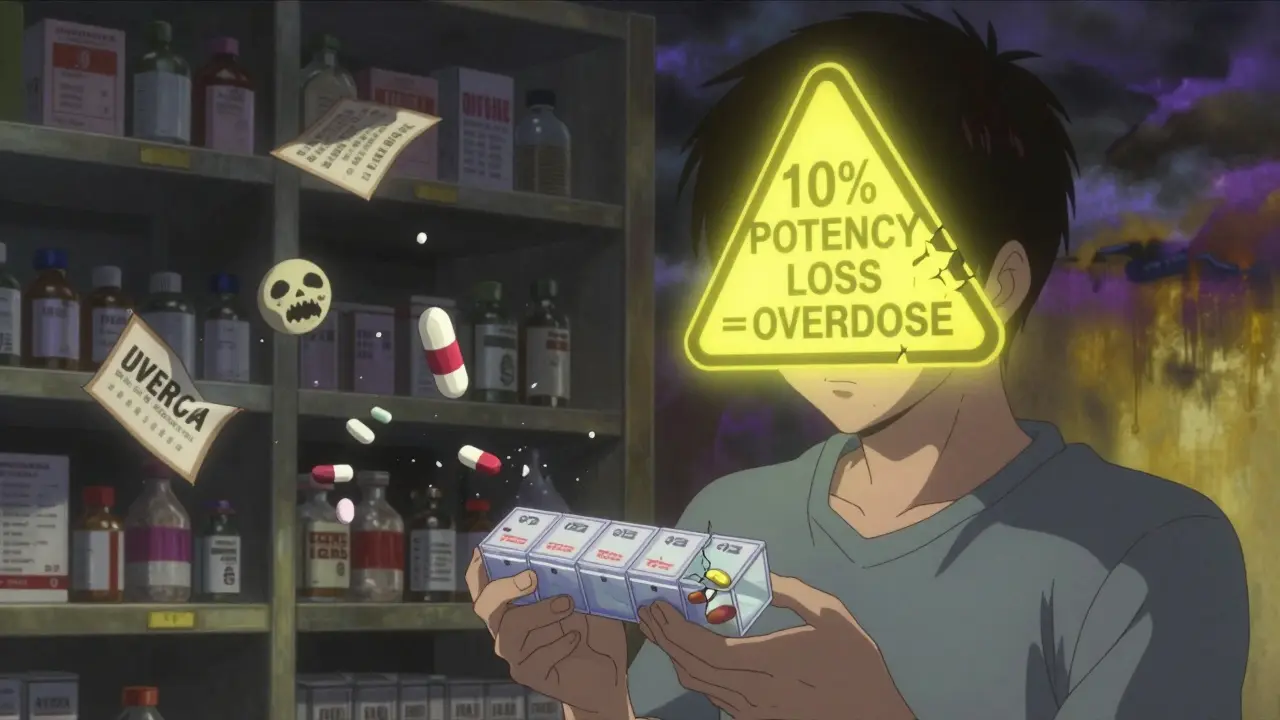
The pill you got from the pharmacy was designed to last for months, even years, in its original container. That container? It’s not just plastic or glass. It’s a precision-engineered system with moisture barriers, light-blocking materials, and desiccants built in. Take that same pill and put it in a standard pharmacy vial or a plastic pill organizer, and you’re exposing it to air, humidity, and light it was never meant to handle. The FDA’s Q1A(R2) guidelines make it clear: stability data is tied to the original packaging. When you repack, you break that link. A 2019 study in the Journal of Pharmaceutical Sciences showed albuterol sulfate tablets lost over 15% of their potency in 90 days when stored in standard pharmacy vials. In the original HDPE bottle with a desiccant? Only 3.2% degradation. That’s a fivefold difference. And it’s not just about potency. Degradation can create harmful byproducts. Hydrolysis from moisture, oxidation from air, photodegradation from light-these aren’t theoretical risks. They’re measurable. The USP says container-closure systems must protect the drug. Most repackaging containers don’t meet that standard.What Happens Inside a Pillbox Over Time
Pillboxes are the worst offenders. They’re often made of cheap plastic, lack seals, and are left on bathroom counters or kitchen tables-places with high humidity and fluctuating temperatures. When you throw amoxicillin, nifedipine, and atenolol into the same compartment, you’re not just organizing your meds-you’re creating a chemical lab. A 2022 study by the American Pharmacists Association found that 18.7% of multi-drug pillboxes showed physical changes within two weeks. Caking. Discoloration. Clumping. These aren’t just cosmetic. They signal chemical reactions. Amoxicillin, for example, breaks down rapidly in moisture. In a humid environment, it can degrade into allergenic compounds. Nifedipine, a light-sensitive calcium channel blocker, turns brown and loses effectiveness when exposed to daylight-even through a translucent pillbox. And here’s the scary part: most people don’t know. The Institute for Safe Medication Practices (ISMP) reported in 2020 that 32% of community pharmacies had no formal stability protocols for repackaged meds. That means your pillbox might be full of drugs that are half-dead-or worse, toxic.How to Actually Test Stability (Without a Lab)
You don’t need an HPLC machine to spot danger. You just need to know what to look for.- Color changes: If a white tablet turns yellow, brown, or gray, toss it. That’s oxidation or hydrolysis in action.
- Texture changes: Tablets that crumble, stick together, or feel oily are degraded. Solid oral dosage forms shouldn’t change feel.
- Odor: If your meds smell sour, musty, or chemical, they’ve reacted with moisture or air. This is especially common with antibiotics like amoxicillin.
- Moisture signs: Condensation inside the container? Desiccant pack soaked through? That’s a red flag. Even if the pills look fine, moisture has breached the barrier.

What the Experts Say About Shelf Life
The FDA doesn’t set expiration dates for repackaged meds. Pharmacies do. And they’re supposed to base those dates on real data, not guesswork. The International Pharmaceutical Federation (FIP) recommends a maximum of 6 months for repackaged solid oral drugs under normal conditions. But that’s the ceiling. Most drugs need far less.- Amoxicillin and other hygroscopic antibiotics: 30 days max. Moisture kills them fast.
- Nifedipine, nitroglycerin, isosorbide: 60 days. Light-sensitive. Use amber vials.
- Atenolol, lisinopril, metformin: 90 days. Relatively stable, but still degrade over time.
- Any drug with a desiccant in the original bottle: Never repack without adding a new desiccant pack. It’s not optional.
How Pharmacies Should Handle This (And Why Most Don’t)
The ASHP and USP have clear guidelines: repackaged meds need stability testing. For high-risk drugs, that means HPLC analysis. For others, accelerated testing at 40°C and 75% humidity for 14 days can predict long-term stability. But here’s the gap: only 28% of independent pharmacies have HPLC equipment. Most rely on manufacturer data, which is useless for repackaged products. That’s why the FDA issued a warning letter in 2023 to a major pharmacy chain for failing to assign expiration dates properly-and shut them down for 45 days. The solution? A tiered approach:- High-risk drugs: Test with HPLC or use a validated database like the University of Florida’s.
- Low-risk drugs: Use bracketing-group similar drugs (e.g., all beta-blockers) and assign expiration based on the least stable one.
- Always: Use desiccant packs in repackaged containers. A 2023 multicenter trial showed this extended stability by 47%.
What You Can Do Right Now
You don’t have to be a pharmacist to protect yourself.- Ask your pharmacy: “What’s the expiration date for this repackaged med, and how was it determined?” If they say, “It’s the same as the bottle,” walk out.
- Never use a pillbox longer than 30 days for antibiotics, heart meds, or thyroid drugs.
- Store pillboxes in a cool, dry place-not the bathroom or near the stove.
- Check for desiccant packs. If it’s missing, ask for a new container.
- Throw out anything that looks, smells, or feels wrong. Don’t wait for the date.
What’s Changing in 2025
The USP is finalizing <1790> Repackaged Drug Product Stability in early 2025. This will require:- Minimum 12 units tested per timepoint
- At least 3 testing points for meds used under 90 days
- Container integrity testing using vacuum decay or helium leak detection
Can I trust the expiration date on a repackaged medication?
No. The expiration date on the original bottle applies only to the drug in its original container. Once it’s repackaged, that date is invalid. Pharmacies must assign a new expiration date based on stability testing. If they don’t, the date is meaningless-and potentially dangerous.
How long can I keep meds in a pillbox?
For most medications, 30 days is the safest limit. High-risk drugs like antibiotics, blood thinners, or seizure medications should not be kept longer than 14-30 days. Light-sensitive or moisture-sensitive drugs (like nifedipine or amoxicillin) degrade quickly. If your pillbox is full for more than a month, it’s time to refill and inspect.
Is it safe to repack medications myself at home?
It’s not recommended. Home environments lack controlled humidity, temperature, and clean conditions. You can’t replicate the barrier protection of pharmaceutical-grade containers. Even a small amount of moisture can degrade pills. If you need help organizing meds, ask your pharmacist to use a proper repackaging system with desiccants and labeled expiration dates.
What should I do if my meds look or smell different?
Throw them away immediately. Discoloration, caking, crumbling, or unusual odors are signs of chemical degradation. Don’t assume they’re still safe. Degraded medications can be ineffective-or even toxic. Contact your pharmacist to get a replacement and report the issue.
Do desiccant packs really help?
Yes. A 2023 study involving over 8,400 repackaged units showed that adding a desiccant pack extended stability by 47%. For moisture-sensitive drugs like amoxicillin or albuterol, this can be the difference between a safe dose and a failed treatment. Always check that a desiccant is included-and replace it if it’s wet or missing.