When depression doesn’t respond to the first antidepressant you try, it’s not necessarily a failure-it might just mean your brain needs a different kind of support. That’s where SNRI medications come in. Unlike older antidepressants that target just one neurotransmitter, SNRIs work on two: serotonin and norepinephrine. This dual action makes them uniquely useful for people who struggle with depression plus fatigue, brain fog, or chronic pain. They’re not the first thing doctors reach for, but for many, they’re the one that finally works.
What SNRIs Actually Do in Your Brain
SNRIs stand for Serotonin and Norepinephrine Reuptake Inhibitors. That’s a mouthful, but here’s what it means in plain terms: your brain uses serotonin and norepinephrine to regulate mood, energy, focus, and even pain signals. After these chemicals do their job, they’re usually sucked back up into the nerve cells that released them. SNRIs block that reabsorption, so more of these mood-boosting chemicals stay active in the spaces between brain cells.
This isn’t just theory. Clinical studies show that SNRIs increase the availability of both neurotransmitters right from the start, unlike some older drugs that only affect serotonin at low doses. Duloxetine and levomilnacipran, for example, hit both targets equally from day one. Venlafaxine, on the other hand, starts by focusing on serotonin and only ramps up norepinephrine inhibition at higher doses-around 150mg per day or more.
That’s why SNRIs aren’t just for sadness. They’re used for anxiety, fibromyalgia, diabetic nerve pain, and even long-term back pain. If you’ve been told your pain is "all in your head," but you still feel it in your bones-that’s where SNRIs can help. The brain’s pain pathways use the same chemicals as mood regulation, so boosting them can ease both.
The Four Main SNRIs You’ll Actually See
There are four SNRIs approved in the U.S. for depression and other conditions:
- Venlafaxine (Effexor XR): The original SNRI, approved in 1993. Often used for depression and generalized anxiety. Comes in extended-release form to reduce side effects.
- Duloxetine (Cymbalta, Drizalma Sprinkle): The most versatile. Approved for depression, anxiety, fibromyalgia, diabetic neuropathy, and chronic musculoskeletal pain. Also approved for kids 7+ with anxiety.
- Desvenlafaxine (Pristiq): A metabolite of venlafaxine. Often prescribed when venlafaxine causes too many stomach issues.
- Levomilnacipran (Fetzima): The newest. May be more effective for fatigue and low energy than others.
Each has slightly different dosing. Duloxetine usually starts at 30mg and goes up to 60-120mg. Venlafaxine XR often begins at 37.5mg and can go as high as 225mg. Dosing isn’t one-size-fits-all-it’s adjusted slowly over weeks to find the sweet spot between effect and side effects.
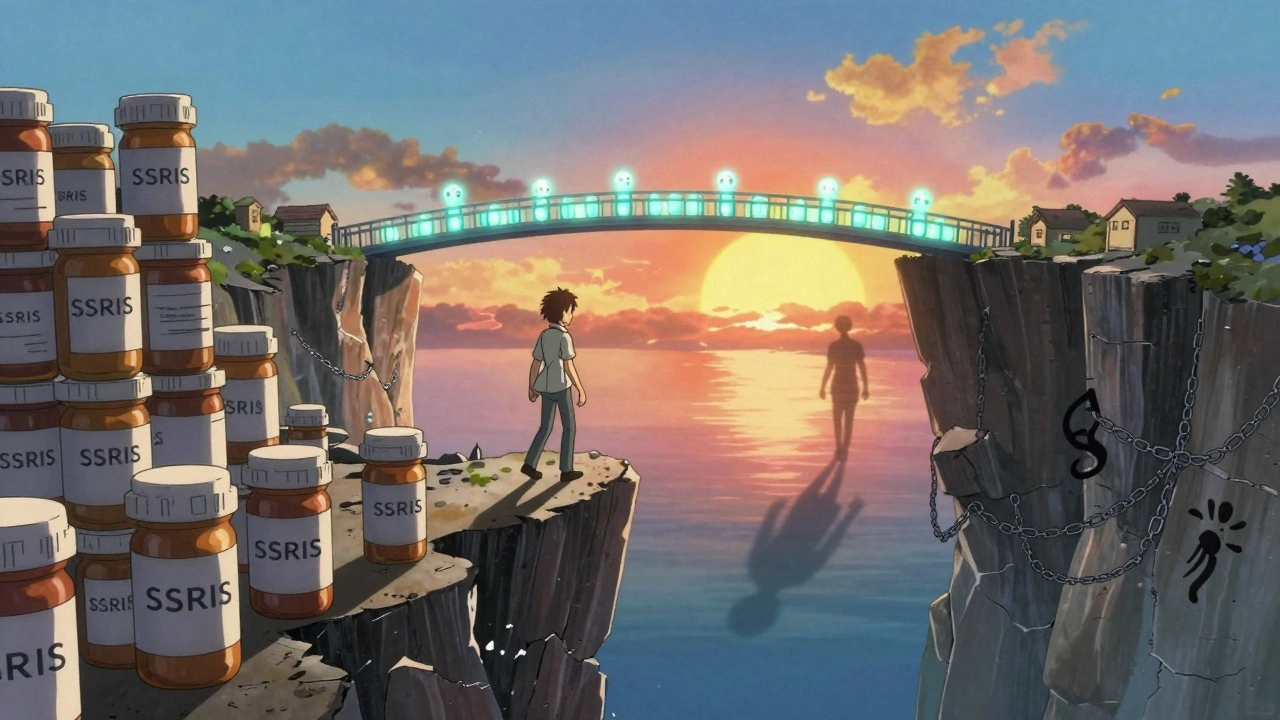
How SNRIs Compare to SSRIs
SSRIs like sertraline or escitalopram are still the go-to first-line antidepressants. Why? They’re gentler. Fewer side effects. Easier to start. But they don’t always do enough.
Studies show SSRIs help about 50-60% of people with depression. SNRIs help 55-65%. That 5-10% difference might not sound like much, but for someone who’s tried three SSRIs and still feels numb, it’s everything. The real advantage? SNRIs work better when depression comes with physical symptoms-fatigue, slow thinking, muscle aches, or nerve pain.
A 2022 meta-analysis found that duloxetine reduced pain by 30-50% in 40-50% of patients with diabetic neuropathy. Placebo? Only 20-30% saw any relief. That’s not a small win. It’s life-changing for people who’ve been told their pain is "just aging" or "stress-related."
For pure depression without physical symptoms, SSRIs are still preferred. But if you’re exhausted, can’t concentrate, and your shoulders ache all day? SNRIs are often the better fit.
Side Effects: What to Expect
No antidepressant is side-effect-free. SNRIs are no exception. The most common ones:
- Nausea: Happens in about 25% of people, especially in the first two weeks. Usually fades. Taking it with food helps.
- Dizziness: Around 15-20%. Often linked to blood pressure changes.
- Insomnia or sleepiness: Some feel wired; others feel sluggish. Timing the dose (morning vs. night) can help.
- Sexual side effects: Lowered libido, delayed orgasm, or erectile dysfunction. Affects 20-30% of users-similar to SSRIs.
- Blood pressure rise: Happens in 2-3% of users. Not everyone. But doctors check BP at 2-4 week intervals early on.
Compared to older tricyclic antidepressants, SNRIs are much safer. Tricyclics cause dry mouth in up to 50% of users, constipation, blurry vision, and heart rhythm issues. SNRIs rarely cause those.
But here’s the big one: discontinuation syndrome. If you stop SNRIs suddenly, you can get brain zaps (electric shock sensations), dizziness, nausea, anxiety, or flu-like symptoms. That’s because your brain has adapted to the higher levels of serotonin and norepinephrine. Stopping fast throws it off balance.
Studies show tapering slowly over 4-6 weeks cuts the risk of withdrawal from nearly 30% down to under 10%. Never quit cold turkey-even if you feel fine.
Real People, Real Results
Online forums like Reddit’s r/mentalhealth have thousands of stories. One user wrote: "I tried four SSRIs. Nothing worked. I felt like a zombie. Then I started duloxetine. Within six weeks, I could get out of bed. My fibromyalgia pain dropped by half. I haven’t cried in months."
Another said: "I loved the energy boost from venlafaxine-but the nausea was brutal for three weeks. My doctor lowered the dose, then slowly increased it. Now I’m stable."
On Drugs.com, duloxetine has a 6.1/10 rating. The top positive reviews mention: "Finally worked after 3 failed antidepressants," and "My pain is manageable." The top complaints? "Withdrawal was hell," and "I couldn’t tolerate the nausea."
Here’s the thing: SNRIs don’t work for everyone. But for those who’ve tried other meds and still struggle? They’re often the breakthrough.
How Doctors Start and Monitor SNRIs
Doctors don’t just hand you a prescription and say "good luck." There’s a process:
- Start low: Usually 37.5mg of venlafaxine XR or 30mg of duloxetine daily. This reduces nausea and dizziness.
- Wait and watch: Give it 4-6 weeks before deciding if it’s working. Some need 8-12 weeks.
- Titrate slowly: Increase dose every 4-7 days if needed. No rushing.
- Check blood pressure: Especially in the first month. If BP goes above 140/90, your doctor may adjust the dose or switch meds.
- Combine with therapy: A 2022 trial found 73% of people on SNRIs + CBT reached remission. Only 48% did with medication alone.
For chronic pain, doctors often start at the same dose as for depression. No need to wait for mood to improve before seeing pain relief-it often happens sooner.
What’s New and What’s Next
The SNRI field isn’t standing still. In 2022, the FDA approved Drizalma Sprinkle-duloxetine in granule form that can be mixed with soft food. It’s a game-changer for kids or people who can’t swallow pills.
Genetic testing is becoming more common. Some people metabolize SNRIs too fast or too slow because of their CYP2D6 or CYP2C19 genes. Testing can help avoid trial-and-error. It’s not perfect yet, but it’s getting better.
Researchers are also testing SNRIs combined with digital tools. A 2023 study showed that people taking duloxetine plus a cognitive training app improved memory and focus 35% more than those on the drug alone.
And while psychedelic therapies like ketamine are getting attention for treatment-resistant depression, SNRIs still hold their ground. They’re oral, affordable, and backed by decades of data. For now, they’re the most reliable second-line option.
Who Should Avoid SNRIs?
Not everyone is a candidate. Avoid SNRIs if you:
- Have uncontrolled high blood pressure
- Take MAO inhibitors (like phenelzine) or have taken them in the last 14 days
- Have liver disease (duloxetine is processed by the liver)
- Are pregnant or breastfeeding-data is limited, so risks must be weighed
- Have a history of mania or bipolar disorder (SNRIs can trigger mania)
And yes-there’s a black box warning for increased suicidal thoughts in people under 25. That’s true for all antidepressants. It’s rare, but your doctor should check in closely during the first few weeks.
Bottom Line: Are SNRIs Right for You?
If you’ve tried an SSRI and still feel stuck-fatigued, foggy, in pain-SNRIs might be your next step. They’re not magic. They take time. They have side effects. But for many, they’re the missing piece.
They’re not for everyone. But for those who’ve been told "you’re just depressed" when they felt like their whole body was heavy, slow, and hurting? SNRIs offer something deeper than just lifting mood. They help you feel alive again.
How long does it take for SNRIs to start working?
Most people start noticing small improvements in energy or mood after 2-4 weeks, but full effects usually take 4-6 weeks. Some need up to 12 weeks, especially for pain relief. Patience is key-don’t stop too soon.
Can SNRIs help with chronic pain even if I’m not depressed?
Yes. Duloxetine and venlafaxine are FDA-approved for diabetic neuropathy, fibromyalgia, and chronic musculoskeletal pain-even without depression. They work by calming overactive pain signals in the brain and spinal cord.
Do SNRIs cause weight gain?
Unlike some antidepressants, SNRIs are less likely to cause weight gain. In fact, some people lose a little weight early on due to reduced appetite or nausea. Long-term weight changes vary by person, but significant gain isn’t common.
What’s the difference between venlafaxine and duloxetine?
Venlafaxine works more like an SSRI at low doses and becomes a full SNRI at higher doses. Duloxetine balances both neurotransmitters from the start. Duloxetine is also approved for more pain conditions and has a pediatric indication for anxiety. Venlafaxine is often cheaper as a generic.
Can I drink alcohol while taking SNRIs?
It’s best to avoid alcohol. It can worsen dizziness, drowsiness, and liver strain. It also increases the risk of high blood pressure and may interfere with mood improvement. A glass now and then might be okay, but talk to your doctor first.
What happens if I miss a dose?
If you miss a dose, take it as soon as you remember-unless it’s close to your next dose. Don’t double up. Missing doses can trigger withdrawal symptoms like brain zaps or nausea. Use a pill organizer or phone reminder to stay on track.
If you’re considering SNRIs, talk to your doctor about your full symptom picture-not just mood, but energy, sleep, and pain. The right medication isn’t about being "depressed"-it’s about finding what helps your whole system work again.