SNRI Medications: What They Are, How They Work, and What You Need to Know
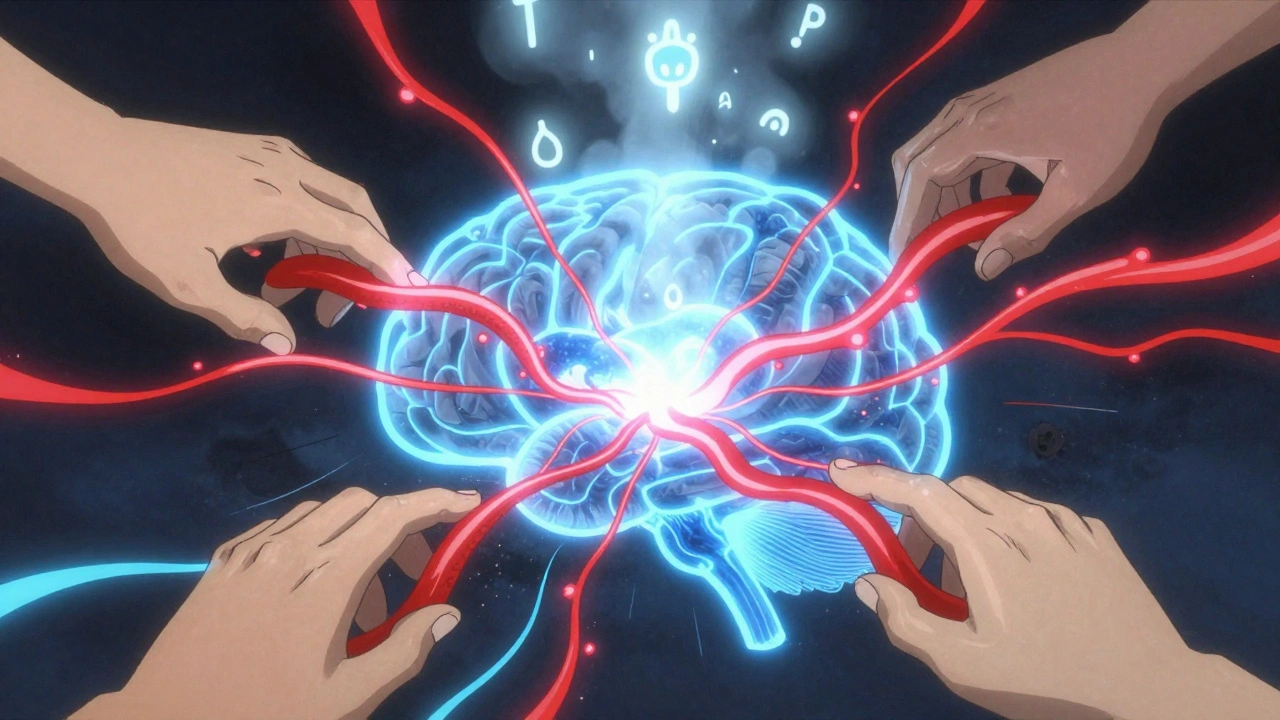
When you hear SNRI medications, a class of antidepressants that increase serotonin and norepinephrine levels in the brain. Also known as serotonin-norepinephrine reuptake inhibitors, they’re commonly prescribed for depression, anxiety, and chronic pain. Unlike older antidepressants, SNRIs don’t just boost one chemical—they target two, which can make a difference for people who don’t respond to SSRIs alone.
These drugs include venlafaxine, duloxetine, and desvenlafaxine. Each works slightly differently, but they all block the reabsorption of serotonin and norepinephrine, keeping more of these mood-regulating chemicals active in your brain. That’s why they’re used not just for depression, but also for nerve pain, fibromyalgia, and even some types of incontinence. But here’s the catch: they don’t work the same for everyone. Some people feel better fast. Others notice side effects like nausea, dizziness, or sleep changes before the benefits kick in. And if you’re already taking other meds—like opioids, migraine drugs, or even certain herbal supplements—you could be at risk for something called serotonin syndrome, a rare but dangerous condition caused by too much serotonin in the body. It’s not common, but it’s serious. Symptoms include rapid heart rate, high blood pressure, confusion, muscle stiffness, and fever. If you’re on an SNRI and start feeling off, don’t wait—talk to your doctor.
Another thing to watch: SNRIs can interact with other medications that affect how your liver processes drugs. For example, if you’re taking something like ritonavir for HIV or certain antibiotics, your body might not clear the SNRI properly, leading to higher levels in your blood. That’s why it’s not just about the drug itself—it’s about the whole mix. And if you’ve ever had a bad reaction to an SSRI, you might react similarly to an SNRI. That’s not a guarantee, but it’s a signal to move slowly and monitor closely.
Many people stop SNRIs too soon because they don’t feel better right away. But these meds often take 4 to 6 weeks to show real results. Side effects usually fade as your body adjusts. Still, if you’re thinking about quitting, don’t just stop. Tapering off under a doctor’s care prevents withdrawal symptoms like brain zaps, dizziness, or mood swings. And if you’re pregnant, breastfeeding, or managing another health condition, your options might be narrower than you think. That’s why the best decisions come from talking through your full picture—not just your symptoms.
Below, you’ll find real-world stories and science-backed guides on how SNRIs fit into broader medication safety. From drug interactions that can turn dangerous to how serotonin syndrome shows up in everyday life, these posts help you spot risks before they become emergencies. You’ll also see how SNRIs compare to other antidepressants, what to do if side effects don’t go away, and why some people need to avoid them entirely. This isn’t theory. It’s what people actually experience—and what their doctors wish they’d known sooner.