Every year, more than 1.5 million people in the U.S. end up in the emergency room because of mistakes with their medications. These aren’t rare accidents. They’re systemic failures - and they’re preventable. Medication safety isn’t just about pharmacists double-checking labels. It’s about whether your entire healthcare system is designed to keep you alive when you take a pill, get an injection, or use an infusion pump. When medication safety fails, people die. And it’s happening more often than most realize.
Medication Errors Are a Leading Cause of Harm
The World Health Organization calls unsafe medication practices one of the top causes of injury in healthcare. In high-income countries, one in every ten patients suffers harm from a medication error. In lower-resource settings, it’s one in twenty. That’s not a glitch. That’s a pattern. And the cost? Over $42 billion globally each year. In the U.S. alone, medication non-adherence - people not taking their drugs as prescribed - leads to 125,000 preventable deaths annually and adds $300 billion to healthcare spending. These aren’t abstract numbers. They’re mothers forgetting their blood pressure pills because the instructions were unclear. Elderly patients mixing up their diabetes and heart meds because the bottles look too similar. Nurses giving the wrong dose because the electronic system didn’t flag a dangerous interaction. A 78-year-old man in Ohio died after an infusion pump delivered ten times the intended dose of pain medication. The machine didn’t malfunction - it was programmed wrong, and no one caught it.The Growing Threat of Fake and Dangerous Drugs
It’s not just mistakes in hospitals or pharmacies. The drug supply chain is under siege. In 2023, the DEA seized over 80 million counterfeit pills laced with fentanyl. Fentanyl is now the leading cause of death for Americans between 18 and 45. Many of these pills are sold as oxycodone or Xanax, but they’re deadly. They’re not rare. They’re everywhere - bought online, handed out at parties, even found in some community pharmacies. The problem isn’t just street drugs. Even legal prescriptions are at risk. The FDA’s MAUDE database recorded over 200 deaths and 1,900 injuries from faulty infusion pumps between January 2023 and August 2024. Many of these weren’t due to user error. They were caused by software bugs, poor screen design, or lack of safety alerts. One nurse in Pennsylvania told a reporter she once programmed a pump to deliver insulin at 10 units per hour. The system accepted it. The patient’s blood sugar dropped to zero. She survived. Others didn’t.Technology Can Help - But Only If It’s Used Right
There are proven solutions. Barcode scanning at the bedside cuts administration errors by 86%. Electronic health records with built-in alerts reduce prescribing mistakes by 55%. Pharmacist-led medication reviews increase adherence by 40% and save $1,200 per patient per year. The Mayo Clinic used AI to reconcile medications at discharge and slashed post-hospital errors by 52%. Geisinger Health’s pharmacist program cut readmissions by 27%. But technology alone won’t fix this. Only 63% of U.S. hospitals had fully compliant electronic systems in late 2024, even though federal rules required it. Many systems still don’t talk to each other. A patient discharged from a hospital might get a list of five new meds. Their primary care doctor has no access to that list. Their pharmacist doesn’t either. That’s how errors slip through.
The Real Problem: Systems Over People
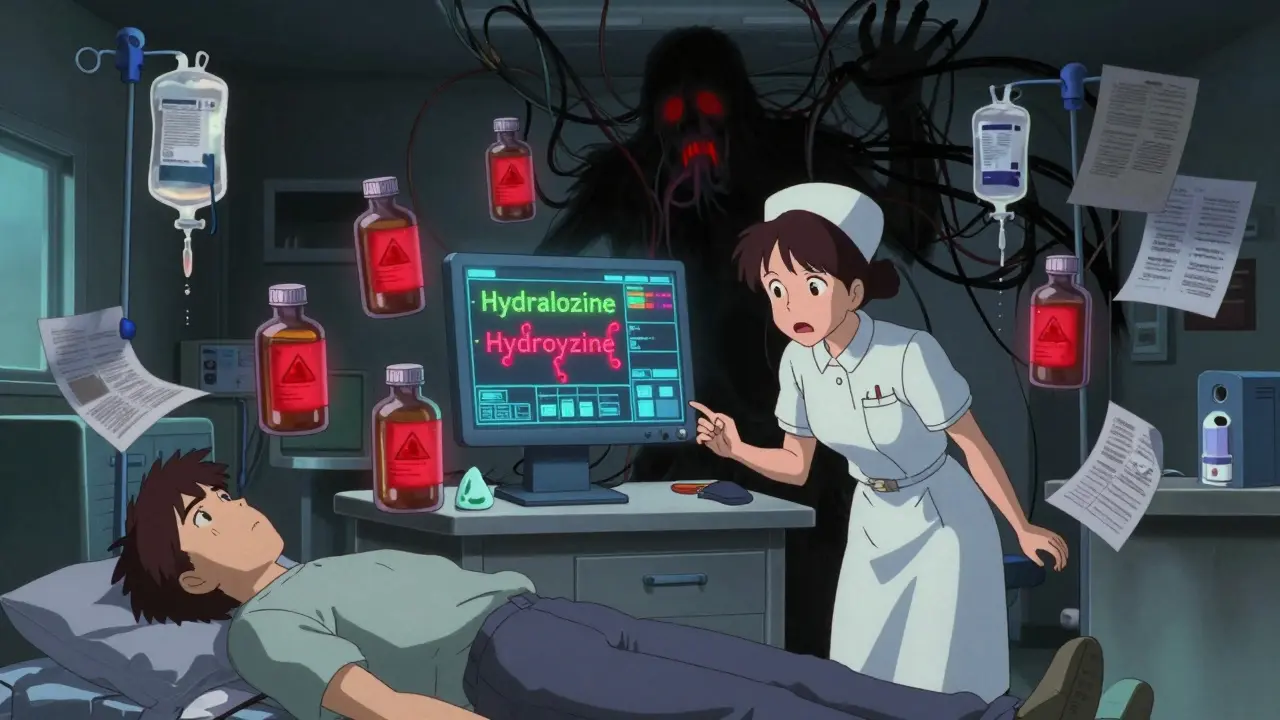
Most people think medication errors happen because someone’s tired or careless. But research shows 89% of errors come from flawed systems - not human failure. Look-alike drug names. Confusing EHR interfaces. Lack of standardized protocols during transitions of care. A 2024 study of 15,000 patient handoffs found that two-thirds had at least one unintentional medication change - a new drug added, an old one stopped, a dose changed - without anyone telling the patient or their doctor. Nurses report near-misses every month because two drugs sound alike: “Hydralazine” and “Hydroxyzine.” One treats high blood pressure. The other treats anxiety. Mix them up, and you could trigger a heart attack. Pharmacists intercept these mistakes - but they shouldn’t have to be the last line of defense.How Other Countries Are Getting It Right
The Netherlands reduced medication errors by 44% by making electronic prescribing mandatory across all healthcare settings - hospitals, clinics, pharmacies, even home care. Everyone uses the same system. No paper. No faxes. No guesswork. The UK’s National Reporting and Learning System collects every medication error, no matter how small. They analyze trends, share lessons, and update protocols. As a result, serious errors dropped by 30%. In the U.S., reporting is voluntary. Only 14% of errors are ever documented. That means we’re flying blind. We don’t know the full scope. We can’t fix what we won’t measure.
What Needs to Change - Right Now
Here’s what works, based on real data:- Standardize medication reconciliation at every transition - admission, discharge, transfer. No exceptions.
- Make barcode scanning mandatory for all medications in hospitals. It’s not optional anymore.
- Require pharmacist involvement in discharge planning. Not as a formality - as a core part of care.
- Implement patient-facing portals where people can see their full med list, get alerts about interactions, and ask questions.
- Enforce national reporting of all medication errors. No more hiding behind state-by-state rules.
Why This Matters to Everyone
You might think, “I’m healthy. This doesn’t affect me.” But it does. When medication safety fails, it drives up costs for everyone. Insurance premiums rise. Taxes go up. Hospitals spend more on treating preventable harm than on prevention. And it’s not just about pills. It’s about trust. If you can’t trust that the medicine your doctor prescribes won’t kill you, why go to the doctor at all? The good news? Every dollar invested in medication safety returns $7.50 in savings. Pharmacist-led programs return $13.20 for every dollar spent. We know what works. We have the tools. We just need the will.What You Can Do
You don’t have to wait for the system to fix itself.- Keep a written list of every medication you take - including doses, times, and why you take them.
- Ask your pharmacist: “Are any of these drugs dangerous to take together?”
- At discharge, demand a full medication review with your doctor and pharmacist - together.
- Use apps or paper charts to track your meds. Don’t rely on memory.
- Report any confusion, near-misses, or errors - to your provider, to the hospital, to the FDA.
Medication safety isn’t a luxury. It’s the bare minimum. If we can’t get this right, we shouldn’t be calling ourselves a healthcare system. We’re not just treating disease. We’re keeping people alive. And that starts with making sure the medicine they take doesn’t hurt them.
What is the most common cause of medication errors in hospitals?
The most common cause isn’t human error - it’s system failure. Poorly designed electronic health records, look-alike drug names, lack of standardized protocols during patient transfers, and disconnected pharmacy and clinical systems are the top culprits. Studies show 89% of medication errors stem from these structural issues, not from nurses or doctors being careless.
How many people die each year from medication errors in the U.S.?
Approximately 125,000 preventable deaths occur annually in the U.S. due to medication non-adherence and errors. This number doesn’t include deaths from counterfeit drugs or infusion pump failures, which add thousands more. The CDC estimates adverse drug events contribute to over 1.5 million emergency room visits each year, many of which are fatal.
Can technology really reduce medication errors?
Yes, when used correctly. Barcode-assisted medication administration reduces errors by 86%. Clinical decision support in electronic health records cuts prescribing mistakes by 55%. AI tools can predict high-risk patients with 73% accuracy. But technology only works if systems are integrated, staff are trained, and alerts aren’t ignored. Many hospitals install these tools but don’t use them effectively.
Why are counterfeit drugs such a big problem now?
Counterfeit drugs are easier to make and harder to trace. Fentanyl, a synthetic opioid 50 to 100 times stronger than morphine, is being pressed into pills that look like oxycodone or Xanax. The DEA seized over 80 million of these fake pills in 2023 alone. They’re sold online, in vending machines, and even in some pharmacies. The Drug Supply Chain Security Act aims to fix this by 2025, but enforcement is still inconsistent.
What’s the return on investment for improving medication safety?
Every $1 invested in medication safety generates $7.50 in healthcare savings. Pharmacist-led interventions return $13.20 for every dollar spent. This comes from fewer hospital readmissions, fewer ER visits, and less waste from incorrect or unused medications. The financial case is clear - medication safety isn’t a cost. It’s a profit center.
How can patients protect themselves from medication errors?
Keep a written, up-to-date list of all your medications - including supplements and over-the-counter drugs. Ask your pharmacist: “Are any of these dangerous together?” At discharge, demand a face-to-face medication review with your doctor and pharmacist. Use a pill organizer. Don’t rely on memory. Report any confusion or near-misses to your provider. You’re your own best safety net.