Bariatric Medication Dose Calculator
How This Tool Works
This calculator helps you determine if your medication needs adjustment after bariatric surgery based on your procedure type and specific drugs. Based on clinical studies from Mayo Clinic and other medical institutions.
Important: Always consult your doctor or pharmacist before making any medication changes. This tool provides general guidance based on clinical data but does not replace professional medical advice.
What Happens to Your Medications After Bariatric Surgery?
After bariatric surgery, your body doesn’t just lose weight-it changes how it absorbs medicine. A pill that worked perfectly before might not work at all after. This isn’t guesswork. It’s science. And it’s happening to hundreds of thousands of people every year.
More than 700,000 bariatric procedures were done globally in 2022. Most were either sleeve gastrectomy or Roux-en-Y gastric bypass (RYGB). These aren’t just stomach reductions. They’re full rebuilds of your digestive system. And that changes everything about how drugs enter your bloodstream.
Why Your Pills Don’t Work the Same Way Anymore
Before surgery, your stomach acid is strong-pH between 1.5 and 3.5. That’s enough to break down most pills. After surgery, especially with RYGB or sleeve gastrectomy, that acid drops. Your new stomach pouch might have a pH of 4.0 to 6.0. That’s closer to water than stomach acid.
That means drugs that need acid to dissolve-like ketoconazole, itraconazole, or even levothyroxine-don’t break down properly. They pass through unchanged. You’re not getting the dose you were prescribed.
Then there’s the physical change. In RYGB, surgeons bypass 100 to 150 cm of your small intestine. That’s a quarter to a third of your entire absorptive surface. If your drug is supposed to be absorbed in that section, it’s gone before it ever gets there.
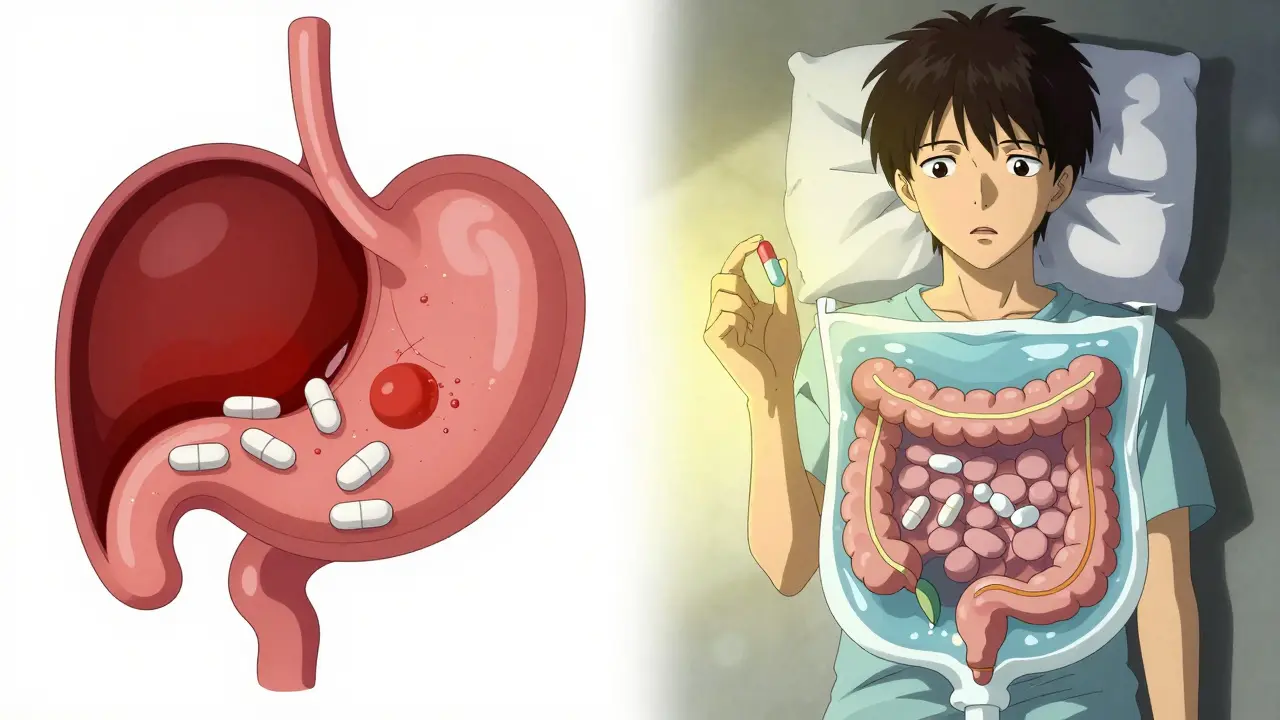
And speed matters. Your stomach empties in 30 to 60 minutes instead of 2 to 5 hours. Pills zip through too fast. Extended-release tablets are designed to release medicine slowly over 8 to 12 hours. But if they’re rushed through your system in 2 hours? They don’t have time to work. Mayo Clinic found that 47% of extended-release medications lost effectiveness after RYGB.
Not All Surgeries Are the Same
Some people think all weight loss surgeries affect drugs the same way. They don’t.
- Sleeve gastrectomy removes 80% of your stomach but leaves the intestines untouched. It raises pH and reduces volume, but absorption is still mostly intact. About 15-20% of drugs show reduced bioavailability. Most people need small tweaks, not full overhauls.
- Roux-en-Y gastric bypass reroutes the digestive tract. This is where things get serious. Up to 68% of patients need medication changes. Drugs like warfarin, levothyroxine, and metformin ER often fail.
- Biliopancreatic diversion bypasses even more intestine. Bioavailability for many drugs drops by 50-70%. This procedure is rare, but the impact is extreme.
- Gastric banding just tightens the stomach. It doesn’t change absorption much-but if you’re eating less, food-dependent drugs like mycophenolate can become ineffective.
The rule of thumb? If your surgery bypasses the duodenum (the first part of the small intestine), expect major changes. If it doesn’t, changes are usually minor.
Drugs That Commonly Fail After Surgery
Some medications are more vulnerable than others. Here are the big ones:
- Levothyroxine: Thyroid hormone. Absorption drops 25-30% after RYGB. Patients often need a 25-50% dose increase. One patient went from 75mcg to 125mcg after surgery.
- Metformin ER: Extended-release diabetes drug. Plasma levels drop 30-40%. Doctors often switch patients to immediate-release versions taken twice daily.
- Glipizide XL: Another diabetes drug. Up to 75% less effective. Many patients end up on insulin instead.
- Oxycodone CR: Long-acting painkiller. Bioavailability drops 60%. Patients report breakthrough pain despite taking the same dose.
- Warfarin: Blood thinner. Dose increases of 25-35% are common in RYGB patients. One study of 217 patients found 60% needed higher doses. Too low? Risk of clots. Too high? Risk of bleeding.
- Extended-release antidepressants: Like sertraline ER or venlafaxine XR. Absorption is unpredictable. Many patients report mood swings or relapse.
- Calcium and vitamin D: Not drugs, but essential supplements. Absorption drops 35%. Almost 72% of patients need higher doses.
These aren’t rare cases. They’re standard outcomes.
What to Do: Practical Steps for Safe Medication Use
You can’t just keep taking the same pills. Here’s what works:
- Switch to immediate-release versions. If you’re on metformin ER, ask for regular metformin taken twice a day. Same with glipizide or oxycodone. Immediate-release forms move through faster and are more predictable.
- Avoid enteric-coated and extended-release pills. These are designed to dissolve in the small intestine. After bypass, they often pass through whole. Patients report pills coming out in their stool-intact.
- Take drugs on an empty stomach. Levothyroxine, for example, absorbs 22% better when taken 30-60 minutes before food after RYGB.
- Use liquids or crushed tablets. For the first 3 months after surgery, liquid forms are preferred. If you must take a pill, crush it (if safe) and mix with water. Check with your pharmacist first-some capsules shouldn’t be opened.
- Get therapeutic drug monitoring. For warfarin, phenytoin, cyclosporine, and other narrow-therapeutic-index drugs, blood tests are non-negotiable. Weekly checks for the first month, then monthly for 3-6 months.
- Track your symptoms. If your pain isn’t controlled, your thyroid feels off, or your mood dips-don’t assume it’s just post-op fatigue. It might be your meds.
What Your Pharmacist Needs to Know
Most community pharmacists have never been trained on this. A 2022 survey found 78% felt unprepared to advise bariatric patients.
Bring your surgical report to the pharmacy. Tell them: “I had a Roux-en-Y gastric bypass” or “I had a sleeve gastrectomy”. That tells them what to look for.
Ask: “Is this medication absorbed in the duodenum or jejunum?” “Is it extended-release?” “Should I switch to a different form?”
Pharmacists who specialize in bariatric care can access dosing calculators now used in 83 U.S. hospitals. These tools factor in your surgery type, weight, and drug profile to suggest accurate doses.
What’s Changing in the Future
This isn’t a static problem. Solutions are evolving.
The FDA added bariatric surgery warnings to 17 drug labels between 2022 and 2023. The European Medicines Agency now requires all new oral drugs to include bariatric absorption data. That’s huge.
New technologies are emerging. pH-adaptive capsules that dissolve in higher pH environments are in trials-and showing 85% absorption in post-surgery patients, compared to 45% for regular pills.
Subcutaneous implants like ITCA 650 (for diabetes) bypass the gut entirely. In one study, they worked in 92% of RYGB patients, while oral versions failed in 32%.
And AI is stepping in. An AI-powered dosing calculator, now used in dozens of hospitals, cut dosing errors by 41% in its first year. It’s not magic-but it’s better than guesswork.
Don’t Wait for Something to Go Wrong
Don’t wait until your pain returns or your blood sugar spikes to act. Medication changes should start before surgery. A 5-step assessment tool used in 127 UK hospitals reduced readmissions by 34% by reviewing all meds pre-op.
Make a list of every pill, supplement, and OTC drug you take. Bring it to your surgeon, endocrinologist, and pharmacist. Ask: “What needs to change?”
And if someone tells you, “It’s probably just your body adjusting”-push back. This isn’t normal healing. This is pharmacology. And it needs a plan.