When you pick up a generic pill at the pharmacy, you’re told it’s the same as the brand-name version. And for the most part, that’s true - the active ingredient is identical. But what you’re not told is that inactive ingredients can be completely different. And for some people, those differences matter a lot more than you’d think.
Think of a pill like a sandwich. The active ingredient is the meat - the part that does the actual work. The rest? That’s the bread, the cheese, the mustard, the pickles. None of those things cure your high blood pressure or ease your thyroid symptoms. But if you’re allergic to mustard, or can’t digest lactose, or react to food dyes? Suddenly, that sandwich isn’t safe anymore. And you didn’t even know you were eating it.
What Are Inactive Ingredients, Really?
Inactive ingredients - also called excipients - are everything in a pill that isn’t the drug itself. They help the medicine hold its shape, dissolve properly, taste better, or last longer on the shelf. Common ones include starches, sugars, dyes, preservatives, and fillers. In some pills, more than 90% of the weight comes from these non-medicinal parts. A single tablet might contain five, ten, or even fifteen different inactive ingredients.
Here’s the catch: while the active ingredient in a generic must match the brand-name drug exactly, manufacturers can use any combination of inactive ingredients they want - as long as the FDA says they’re safe. That means two different generic versions of the same drug could have totally different fillers. One might use lactose. Another might use cornstarch. A third might include a dye that triggers skin rashes in sensitive people.
Why Should You Care?
Most people switch to generics without a problem. But for about 1 in 4 patients, something changes after the switch. A 2022 survey by MedShadow found that 27% of people reported new side effects after switching to a generic. Of those, 68% blamed the inactive ingredients.
People with allergies or intolerances are especially at risk. About 55% of medications contain FODMAP sugars - the kind that cause bloating and cramps in people with IBS. Nearly all pills include at least one common allergen: lactose, gluten, peanut oil, or artificial dyes. And here’s the scary part: there’s no requirement to warn you. If a pill has peanut oil, the label says so. But if it has lactose, modified cornstarch, or sodium metabisulfite? You’re on your own.
One patient in Bristol told her pharmacist she’d had severe stomach cramps every time she switched to generic levothyroxine. She went back to the brand-name version - and the pain vanished. Her doctor had no idea why. The active ingredient was the same. But the filler? Different. And that difference made all the difference.
Real Problems, Real Cases
Studies back this up. A 2017 Harvard study found that after generic versions of blood pressure drugs like losartan and valsartan hit the market, adverse event reports jumped by 8% to 14%. Was it the drug? Or the dye? The preservative? The sugar? No one could say for sure.
People with asthma are another group at risk. Sodium metabisulfite - a common preservative in some generics - can trigger serious breathing problems. The Merck Manual says these are labeled, but only if they’re used in injectables. In pills? Not always.
And it’s not just allergies. If you’re gluten-sensitive, you might not realize that the starch in your generic metformin comes from wheat. If you’re diabetic, the sugar in your generic ibuprofen might spike your blood sugar more than you expect. Even small amounts matter - some allergens cause reactions at levels below a milligram.
Who’s Most at Risk?
You’re more likely to run into problems if:
- You have food allergies or intolerances (lactose, gluten, nuts)
- You have asthma or eczema
- You take five or more medications daily (common in people over 65)
- You’ve had unexplained side effects after switching generics
- You’re on a strict diet (low-FODMAP, keto, paleo)
Over 30% of older adults take five or more pills a day. That means they’re exposed to dozens of different inactive ingredients - and the cumulative effect? Nobody’s studied it properly. One person might tolerate a single pill with lactose. But five pills a day, each with a different sugar? That’s a different story.
What You Can Do
You don’t have to guess. Here’s how to protect yourself:
- Ask your pharmacist - not just for the generic name, but for the full list of inactive ingredients. They can check the manufacturer’s datasheet.
- Check the FDA’s Inactive Ingredient Database - it’s online, but it’s not user-friendly. Look up your drug by brand or generic name and see what fillers are approved.
- Keep a log - write down when you switch generics and what symptoms appear. Did your rash show up after switching to a new bottle? That’s a clue.
- Ask for a brand-name prescription - if you’ve had repeated issues, your doctor can write "dispense as written" or "no substitutions" on the script. Pharmacists must follow that.
- Look for specialty generics - some manufacturers now make "hypoallergenic" versions without common allergens. They’re rarer and cost more, but they exist.
One pharmacy in Bristol started offering a "sensitive formula" option for common drugs like levothyroxine and metformin. It costs a bit more, but for patients with multiple allergies, it’s worth it.
The Bigger Picture
The system was built for efficiency, not individual needs. Generics save the U.S. healthcare system billions each year. But the cost of ignoring patient sensitivity? That’s harder to measure. We know 90% of prescriptions are filled with generics. We also know that 1 in 4 people report side effects after switching. And yet, there’s no standard way to track which fillers are in which pills - or warn patients before they take them.
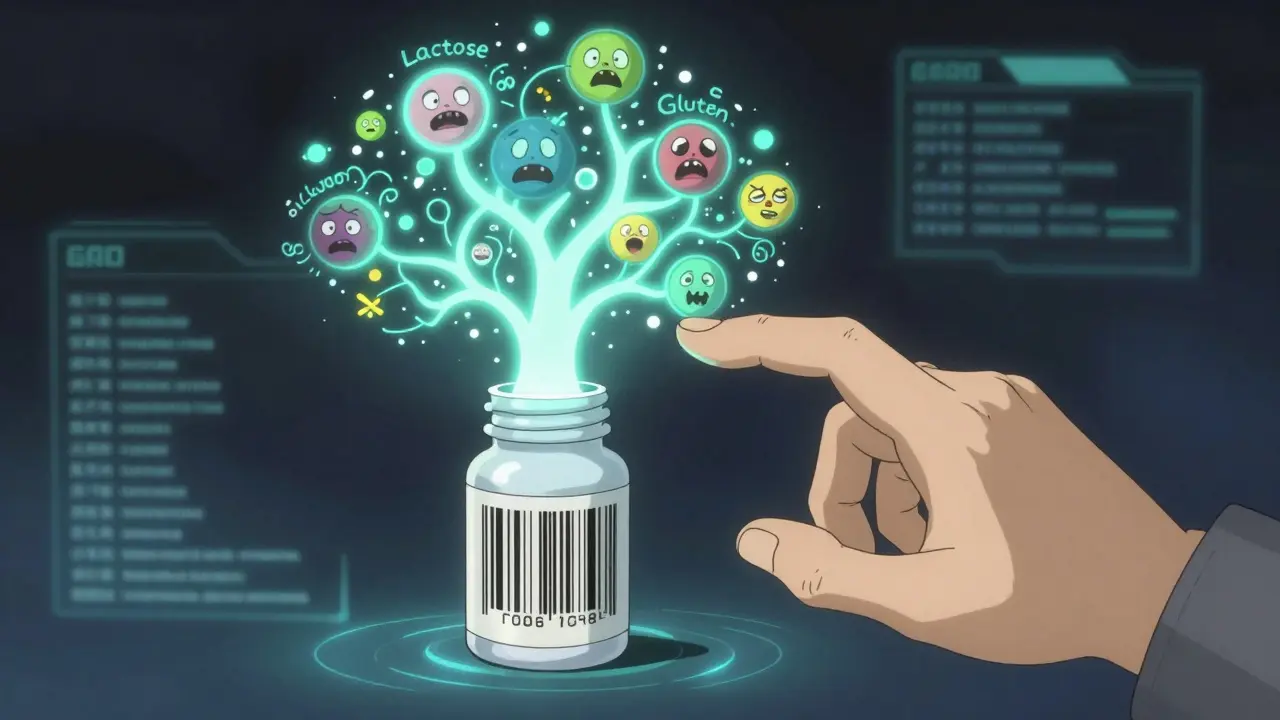
MIT researchers are building a public database that links every generic drug to its exact inactive ingredients. It’s still in testing, but if it goes live, it could change everything. Imagine scanning a barcode on your pill bottle and instantly seeing: "Contains lactose, FD&C Yellow No. 6, and microcrystalline cellulose. May trigger IBS symptoms." That’s not science fiction - it’s coming.
For now, the best tool you have is your own awareness. Don’t assume all generics are equal. Don’t assume your body will react the same way every time. And if something feels off after a switch - trust it. Talk to your pharmacist. Ask for details. Your body is telling you something. Listen.