Steroid-Induced Osteoporosis Prevention Calculator
Your Steroid Details
What Your Body Needs
Daily Recommendations
Why This Matters
Your body needs these nutrients to absorb calcium and maintain bone density while on steroids. Without enough vitamin D, calcium supplements are ineffective.
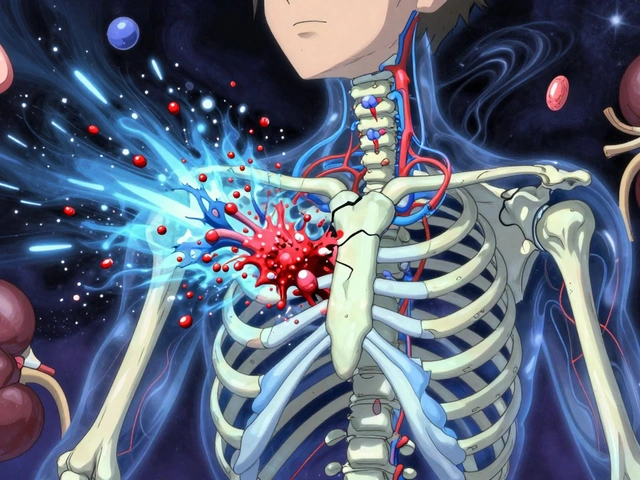
Why Steroids Attack Your Bones
When you take steroids like prednisone for arthritis, asthma, or an autoimmune disease, they don’t just calm your immune system-they also quietly weaken your bones. This isn’t a side effect you hear much about, but it’s one of the most serious. Studies show that 30-50% of people on long-term steroid therapy develop bone loss so severe it leads to fractures. And it happens fast-within just 3 to 6 months of starting treatment.
Here’s how it works: steroids shut down the cells that build new bone (osteoblasts) and turn up the activity of the cells that break bone down (osteoclasts). About 70% of the damage comes from reduced bone building, and 30% from increased bone loss. The result? Your spine and hips become fragile, even if you feel fine. A person on steroids has a 5 to 17 times higher risk of breaking a bone compared to someone their age who isn’t taking steroids.
The Foundation: Calcium and Vitamin D
Before you even think about pills that target bone loss, you need the basics. Every single person starting long-term steroid therapy-no exceptions-should be getting enough calcium and vitamin D. This isn’t optional. It’s the first line of defense.
The American College of Rheumatology recommends 1,000 to 1,200 mg of calcium daily. You can get this from dairy, leafy greens, fortified foods, or supplements. Most people can’t hit that number through diet alone, so supplements are usually needed.
Vitamin D is even more critical. Your body needs it to absorb calcium. Without enough vitamin D, calcium supplements are almost useless. The guideline is 600 to 800 IU daily. If you’re deficient-defined as a blood level below 30 ng/mL-you’ll need 800 to 1,000 IU daily. Many people on steroids are low in vitamin D simply because they’re less active, stay indoors more, or their bodies process it differently.
Don’t just take these and forget them. Get your vitamin D level checked once, especially if you’re over 50 or have darker skin. If you’re low, your doctor may prescribe a higher dose for a few months to bring it up.
Bisphosphonates: The First-Line Shield
If you’re on steroids for more than 3 months at a dose of 2.5 mg or more of prednisone (or its equivalent), and you’re 40 or older, you should be on a bisphosphonate. That’s the standard. And for good reason.
Bisphosphonates like alendronate (Fosamax) and risedronate (Actonel) are the most studied, most used, and most cost-effective drugs for preventing steroid-induced bone loss. They work by slowing down the bone-breakers (osteoclasts). In one major trial, alendronate didn’t just stop bone loss-it actually added 3.7% more bone density to the spine in a year, while the placebo group lost bone.
These drugs are taken orally, once a week. But they’re picky. You have to take them on an empty stomach with a full glass of water, stay upright for at least 30 minutes, and avoid food or other meds for 30 to 60 minutes. Skip these steps and you risk serious irritation in your esophagus. About 15% to 25% of people have trouble with this, which is why many switch to the yearly IV version: zoledronic acid.
Zoledronic acid (Reclast) is given once a year through an IV. It’s just as effective, sometimes more so, and much easier to stick with. In one study, people were 38% more likely to keep taking it than oral bisphosphonates. It’s also better at reducing hip fractures-something oral versions don’t do as well.
When Bisphosphonates Aren’t Enough
Not everyone responds the same. If you’ve already broken a bone, have a very low bone density (T-score below -2.5), or are under 40 with multiple risk factors, bisphosphonates might not be enough. That’s where teriparatide (Forteo) comes in.
Teriparatide is different. Instead of slowing bone loss, it actively builds new bone. It’s a daily injection, and it’s expensive-about $2,500 a month compared to $250 for generic bisphosphonates. But it works better in high-risk cases. In a major study, people on teriparatide had 10 times fewer new spine fractures than those on alendronate.
It’s not for everyone. You can’t use it if you’ve had radiation to your bones, Paget’s disease, or bone cancer. And it’s only approved for 2 years total because long-term safety isn’t fully known. After that, most people switch to a bisphosphonate to maintain the gains.
Another option is denosumab (Prolia), given as an injection every 6 months. It’s effective, especially for people who can’t tolerate bisphosphonates. It’s not first-line yet, but it’s a solid backup.
Monitoring and Timing Matter
You can’t treat what you don’t measure. A bone density scan (DXA) should be done before you start steroids, then again at 12 months. If your bone density drops more than 5% in a year, your treatment needs to change.
Timing is everything. The biggest bone loss happens in the first 6 months. That’s why starting calcium, vitamin D, and a bisphosphonate as soon as you begin steroids is critical. Waiting until you feel pain or get a fracture means it’s already too late.
And here’s the hard truth: only about 1 in 5 patients get their bone density checked within the first year. Many doctors don’t think about it. Many patients don’t know to ask. Don’t be one of them.
What to Avoid
Some things make steroid-induced bone loss worse. Smoking? It cuts bone density. Heavy drinking? Same. Being inactive? Your bones need weight-bearing movement to stay strong. Walking, lifting light weights, even standing more-these help.
Also, don’t rely on over-the-counter supplements without checking doses. Too much calcium (over 2,000 mg/day) can raise your risk of kidney stones. Too much vitamin D (over 4,000 IU/day) can cause high calcium levels in your blood. Stick to the recommended numbers.
What’s Next?
New drugs are coming. Abaloparatide, a newer version of teriparatide, showed better bone growth in trials. Researchers are also testing whether using teriparatide first, then switching to a bisphosphonate, gives better long-term results. But for now, the proven path is clear: calcium, vitamin D, and a bisphosphonate.
Cost is a barrier, but generic alendronate costs less than $10 a month. Zoledronic acid, while pricier per dose, saves money over time because you don’t need to take it every day. And if you’re on Medicare or private insurance, most plans cover these drugs for steroid-induced osteoporosis.
Final Thought: This Isn’t Just About Bones
Preventing steroid-induced osteoporosis isn’t a luxury. It’s part of managing your overall health while on long-term steroids. You’re already taking a powerful drug. You need to protect your body from its hidden damage. Talk to your doctor. Get tested. Start the right supplements. Ask about bisphosphonates. Don’t wait for a fracture to realize how fragile you’ve become.
Can I get enough calcium and vitamin D from my diet alone while on steroids?
It’s very unlikely. Most people need supplements to reach the recommended daily amounts-1,000-1,200 mg of calcium and 600-1,000 IU of vitamin D. Even fortified foods and dairy usually fall short. A blood test for vitamin D levels is the best way to know if you’re deficient.
Do bisphosphonates work for everyone on steroids?
Most people benefit, but not all. People with severe kidney disease (eGFR below 30) can’t take oral bisphosphonates. Those with serious stomach issues may not tolerate them. If you’ve already fractured or have very low bone density, bisphosphonates may not be strong enough-teriparatide or denosumab might be better. Your doctor will assess your risk level.
How long should I stay on bisphosphonates for steroid-induced osteoporosis?
There’s no fixed time. Most people stay on them as long as they’re taking steroids. If your steroid dose drops below 2.5 mg/day for over a year, your doctor might consider stopping. But if you’ve had fractures or very low bone density, you may need to continue longer. Regular bone scans help guide this decision.
Is it safe to take bisphosphonates for years?
Yes, for most people. Long-term use (5+ years) is common and generally safe. Rare risks include atypical femur fractures and osteonecrosis of the jaw, but these affect fewer than 1 in 10,000 people per year. The benefits of preventing spine and hip fractures far outweigh these risks for those on long-term steroids.
Can I take vitamin D and calcium with my steroid pill?
Yes, but timing matters. Take your calcium and vitamin D at a different time than your steroid-ideally, with meals. Avoid taking them together with bisphosphonates, since calcium can interfere with absorption. Always check with your pharmacist or doctor for the best schedule.