Seizure Reduction Calculator
Estimate Your Potential Seizure Reduction
Non-drug therapies can reduce seizure frequency by 30-50% when used appropriately. This calculator helps estimate how different approaches might benefit you based on current research.
Quick Takeaways
- Non‑pharmacological options can cut seizure frequency by 30‑50% when combined with medication.
- Regular aerobic Exercise low‑impact activities that improve cardiovascular health and brain excitability boosts seizure threshold.
- Vagus Nerve Stimulation (VNS) and Responsive Neurostimulation (RNS) are the most evidence‑backed neurostimulation methods for partial onset seizures.
- Ketogenic and Modified Atkins diets supply an alternative metabolic pathway that can stabilize neuronal firing.
- Mind‑body practices-meditation, biofeedback, CBT-target stress, a major seizure trigger.
Understanding Partial Onset Seizures
Partial Onset Seizures are seizures that start in a localized area of the brain and may or may not spread to involve the whole cortex. They account for roughly 60 % of adult epilepsy cases in the United States, according to the CDC’s 2024 epilepsy surveillance report. Symptoms can range from a brief pause in awareness to jerking of a single limb, depending on which cortical region ignites the episode.
Because the electrical storm originates in a specific network, therapies that modulate that network-whether through lifestyle, diet, or targeted neurostimulation-often show meaningful benefit without the side‑effects of anti‑seizure drugs.
Why Look Beyond Medication?
Anti‑seizure medications (ASMs) are the first line of defense, but up to 30 % of patients remain refractory despite trying two or more drugs. Side‑effects such as fatigue, cognitive slowing, and mood changes can erode quality of life. Non‑pharmacological approaches fill two gaps:
- Adjunctive control: they can lower seizure count enough to let patients taper high‑dose ASMs.
- Holistic health: many methods improve sleep, mood, and cardiovascular fitness, which themselves reduce seizure risk.
Choosing the right mix requires a realistic goal‑setting conversation with a neurologist or epileptologist who understands both drug and non‑drug options.
Lifestyle Approaches
Simple daily habits often have the biggest impact because they are easy to sustain.
Exercise
Exercise regular aerobic activity that raises heart rate for 30‑45 minutes, three to five times per week boosts gamma‑aminobutyric acid (GABA) levels, the brain’s chief inhibitory neurotransmitter. A 2023 meta‑analysis of 12 randomized trials showed a 33 % reduction in seizure frequency among participants who added moderate‑intensity cycling or swimming to their routine.
Sleep Hygiene
Sleep Hygiene consistent bedtime routine, dark cool bedroom, and avoidance of caffeine after noon matters because sleep deprivation lowers the seizure threshold. The National Sleep Foundation recommends 7‑9 hours for adults; breaking that into a stable schedule can cut nocturnal seizures by up to 40 %.
Stress Management
Stress spikes cortisol, which can trigger cortical hyper‑excitability. Simple stress‑reduction tactics-progressive muscle relaxation, short walks, or journaling-have been linked to fewer breakthrough seizures in small prospective cohorts.
Dietary Tweaks
Beyond dedicated therapeutic diets, everyday nutrition matters. Low‑glycemic meals prevent rapid glucose swings that could provoke seizures. Incorporating omega‑3‑rich fish, leafy greens, and magnesium‑dense nuts can modestly support neuronal stability.
Mind‑Body Techniques
When the brain’s stress response is the main seizure driver, calming the mind can be powerful.
Meditation & Yoga
Meditation focused attention practices that promote parasympathetic dominance has been studied in a 2022 pilot of 40 adults with refractory partial seizures. Participants meditated 20 minutes daily for eight weeks; average seizure frequency dropped from 6.2 to 3.5 per month.
Biofeedback
Biofeedback real‑time monitoring of physiological signals (e.g., skin conductance) paired with conscious regulation teaches patients to lower sympathetic arousal. Clinical trials report up to a 30 % reduction in seizure count when sessions are combined with relaxation training.
Cognitive Behavioral Therapy (CBT)
CBT helps patients reframe catastrophic thoughts about seizures, which can reduce anxiety‑induced spikes. A 2021 study found that 22 % of CBT participants achieved a ≥50 % seizure reduction, compared with 5 % in the control group.
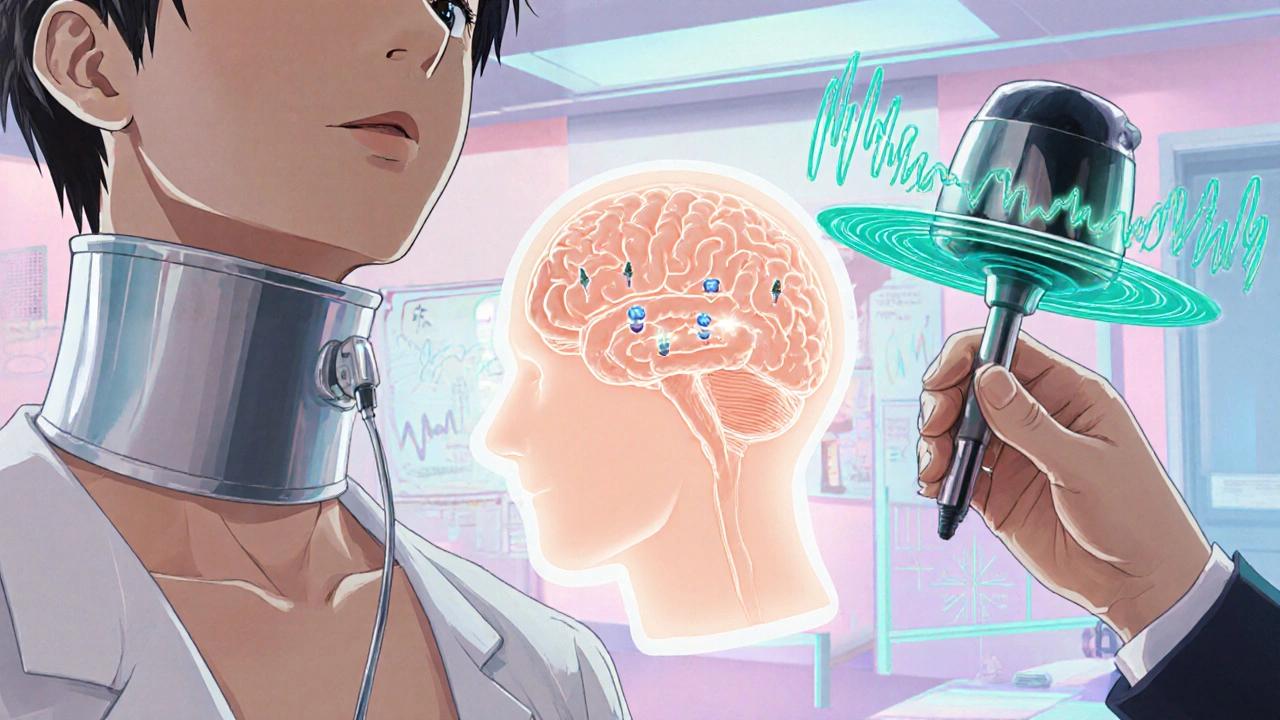
Neuromodulation Options
When lifestyle tweaks aren’t enough, devices that alter brain electrical activity can provide a direct brake on seizure propagation.
| Therapy | Invasiveness | Typical Cost (US) | Best‑Fit Patients | Evidence Level |
|---|---|---|---|---|
| Vagus Nerve Stimulation (VNS) | Implanted neck electrode (minimally invasive) | $30,000‑$45,000 (incl. implantation) | Adults with refractory partial seizures, especially with comorbid mood issues | Level A (multiple RCTs) |
| Responsive Neurostimulation (RNS) | Craniotomically placed leads (moderately invasive) | $45,000‑$55,000 | Patients with a well‑localized seizure focus not amenable to resection | Level A (long‑term safety data) |
| Transcranial Magnetic Stimulation (TMS) | Non‑invasive | $3,000‑$6,000 per course | Patients seeking adjunctive therapy, especially with focal cortical hyper‑excitability | Level B (prospective studies) |
VNS delivers intermittent electrical pulses to the vagus nerve, which then modulates the thalamocortical network. Patients often report mood improvements alongside seizure reduction. RNS, on the other hand, monitors cortical activity in real time and aborts an evolving seizure with targeted stimulation. TMS uses a magnetic coil placed over the scalp to induce a brief electric field; protocols such as low‑frequency (1 Hz) TMS have shown promise in small crossover trials.
Therapeutic Diets
Altering the brain’s fuel source can dramatically affect excitability.
Ketogenic Diet (KD)
Ketogenic Diet high‑fat, low‑carbohydrate regimen that forces the body into ketosis has been a mainstay for children with epilepsy, but adult data are catching up. A 2022 multicenter trial of 120 adults with refractory partial seizures reported a median 38 % reduction in seizure frequency after six months on a classic 4:1 KD.
Modified Atkins Diet (MAD)
The MAD relaxes the strict fat‑to‑protein ratio, making it easier to adhere to. In a prospective cohort of 85 adults, 31 % achieved ≥50 % seizure reduction, and adherence rates were higher than with the classic KD.
Both diets require close monitoring of electrolytes, lipid panels, and kidney function. Partnering with a dietitian familiar with epilepsy nutrition is essential.

Integrating Therapies into a Personalized Plan
No single approach works for everyone. A stepwise framework helps clinicians and patients co‑create a realistic plan:
- Baseline assessment: seizure diary, EEG, medication profile, and comorbidities.
- Lifestyle foundation: implement sleep hygiene, moderate exercise, and stress‑reduction techniques.
- Targeted adjuncts: add a therapeutic diet or neuromodulation device based on seizure focus and patient preference.
- Monitor and adjust: review seizure frequency every 3 months, tweak ASM dose, and modify non‑drug components as needed.
Because many of these strategies are low‑risk, early adoption often yields a “cumulative effect” where each element amplifies the others.
Common Pitfalls & Safety Tips
- Over‑reliance on one method: Combining therapies is usually more effective than any single one.
- Ignoring medication interactions: Some diets (KD) can affect ASM levels; regular blood work is a must.
- Skipping professional guidance: Device implantation or strict diets should never be self‑prescribed.
- Inconsistent tracking: A precise seizure diary helps identify which interventions are truly beneficial.
By staying vigilant and collaborating with a epilepsy specialist, patients can safely explore the full toolbox of non‑pharmacological options.
Frequently Asked Questions
Can non‑drug therapies replace medication completely?
Most adults still need at least one anti‑seizure medication, but many can lower the dose or switch to a less sedating drug after adding lifestyle and dietary changes.
How long does it take to see results from a ketogenic diet?
Clinical trials show a median onset of seizure reduction between 4 and 6 weeks, but maximal benefit often appears after 3-4 months of strict adherence.
Is VNS safe for older adults?
Yes. Studies including participants over 70 years old report comparable seizure reduction and low complication rates, provided the patient has good neck tissue integrity for the cuff.
Do I need a special EEG to qualify for neurostimulation?
A high‑resolution, long‑term video‑EEG is typically required to map the seizure focus, which guides implantation of VNS or RNS leads.
Can stress‑reduction alone reduce seizures?
In mild‑to‑moderate cases, systematic stress management can lower seizure frequency by 20‑30 %. It works best when paired with other interventions.
Exploring non‑pharmacological therapies empowers patients to take an active role in seizure control. By mixing evidence‑backed options-exercise, diet, mind‑body practices, and neuromodulation-most people with partial onset seizures can achieve a more stable, less disruptive life.