When your kidneys start acting up-swelling, fatigue, less urine, weird lab results-it’s easy to blame a UTI or dehydration. But if you’ve been taking common medications like omeprazole, ibuprofen, or an antibiotic for weeks or months, the real culprit might be something far more serious: acute interstitial nephritis (AIN). It’s not rare. It’s not mysterious. And it’s often missed until it’s too late.
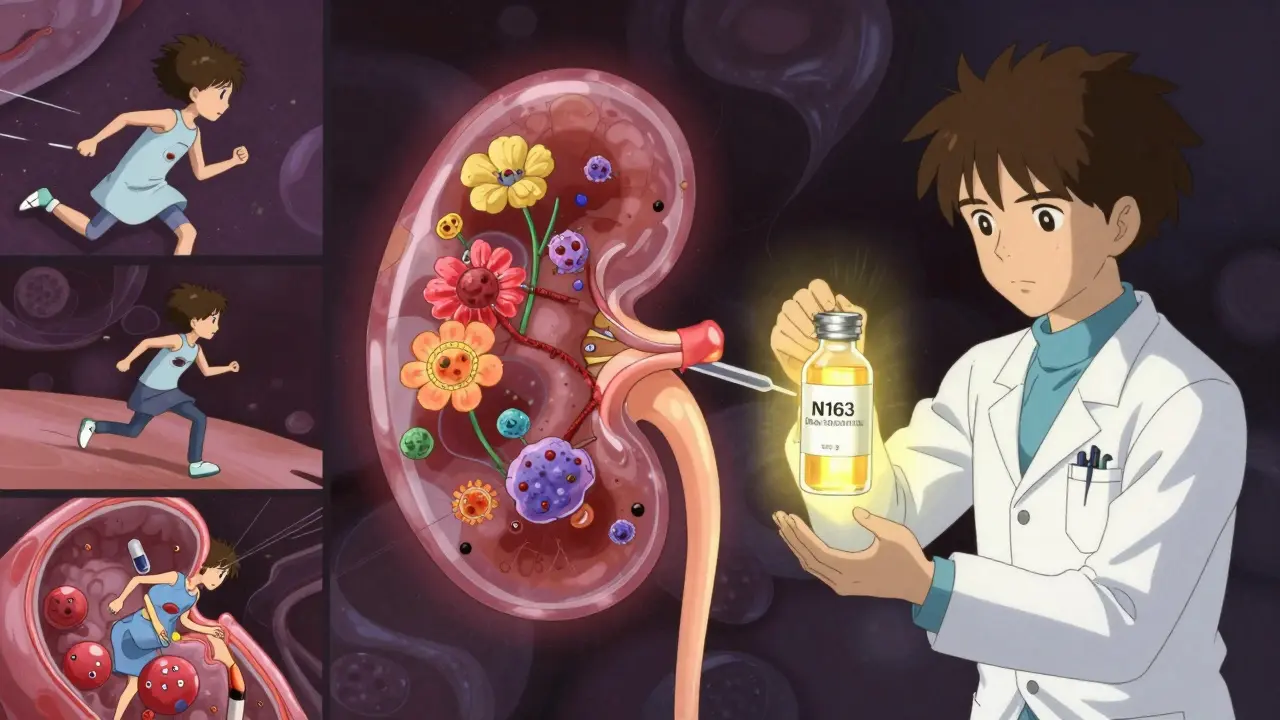
What Exactly Is Acute Interstitial Nephritis?
AIN is inflammation in the spaces between the kidney’s filtering tubes. Think of your kidneys as a network of tiny filters. Between those filters are delicate tissues that help regulate fluid and waste. When drugs trigger an immune reaction, white blood cells flood into those spaces, causing swelling, scarring, and a sudden drop in kidney function. It’s not a slow decline-it’s a sharp turn. Many people end up with acute kidney injury, needing dialysis, or worse, permanent damage.
It’s not caused by infections or toxins alone. In fact, drugs are behind 60-70% of all cases. Over 250 medications have been linked to it. And the list keeps growing. Proton pump inhibitors (PPIs) like omeprazole and pantoprazole are now the second most common trigger-surpassing even antibiotics in recent years. Why? Because millions of people take them daily for heartburn, often for years.
Which Drugs Are Most Likely to Cause It?
Not all drugs are equal when it comes to triggering AIN. The risk, timing, and recovery vary wildly by class:
- NSAIDs (ibuprofen, naproxen, celecoxib): Cause about 44% of drug-induced AIN cases. These are often taken long-term by older adults with arthritis or chronic pain. The damage builds slowly-median time to symptoms is 12 months. Proteinuria can be severe, sometimes reaching nephrotic range. Recovery is slower and less complete than with other triggers.
- Antibiotics (penicillin, amoxicillin, ciprofloxacin, sulfonamides): Account for 33% of cases. These usually hit faster-symptoms show up in about 10 days. Classic signs like rash, fever, and eosinophilia show up in fewer than 10% of people, but skin rashes alone appear in up to half of cases. The good news? Most people recover kidney function fully if caught early.
- PPIs (omeprazole, esomeprazole, lansoprazole): Now the #2 cause. They’re often blamed for mild symptoms, so they’re overlooked. Even though the inflammation is usually less severe, recovery is worse: only 50-60% of patients regain full kidney function. One study showed a 63-year-old woman needed 3 weeks of dialysis after 18 months of daily omeprazole-and still had only 45% kidney function a year later.
- Immune checkpoint inhibitors (used in cancer treatment): An emerging cause. These drugs turn the immune system loose on tumors-but sometimes they turn it on the kidneys too. These cases are growing fast as cancer immunotherapy becomes more common.
The takeaway? It’s not about one drug. It’s about how long you’ve been taking it, how many you’re taking together, and your age. People over 65 are nearly five times more likely to develop AIN than those under 45. And if you’re on five or more medications? Your risk jumps 3.2 times.
What Does AIN Actually Feel Like?
There’s no single symptom. That’s why it’s so often misdiagnosed.
Some people feel nothing at first. Others get:
- Fatigue and nausea
- Fever (low-grade, often missed)
- Joint pain or muscle aches
- Decreased urine output
- Swelling in ankles or face
- Flu-like symptoms that won’t go away
The classic triad-rash, fever, and eosinophilia-shows up in fewer than 10% of cases. So if you’re waiting for a rash to appear before suspecting AIN, you’re already too late. Many patients are told they have a UTI, dehydration, or even the flu. One Reddit thread with 87 AIN-related posts showed 28 people were misdiagnosed as having a urinary infection. That delay? It’s deadly.
How Is It Diagnosed?
There’s no blood test. No urine test. No scan that can confirm AIN for sure.
The only definitive way is a kidney biopsy. A tiny piece of kidney tissue is pulled out with a needle and looked at under a microscope. That’s where doctors see the immune cells, swelling, and sometimes early scarring. It sounds scary-but it’s a quick, low-risk procedure done under local anesthesia.
Other tests help point in the right direction:
- Eosinophiluria (eosinophils in urine): Seen in about half of cases, but not always. False negatives are common.
- 67-gallium scan: Used in the past, but now rarely helpful. It’s outdated and not widely available.
- Urinary CD163: A promising new biomarker. A 2022 study found it detected AIN with 89% accuracy. It’s not standard yet, but it’s the future.
Doctors rely on a combination: recent drug exposure, rising creatinine, absence of other causes, and sometimes a biopsy. If you’ve been on a new medication and your kidney function drops, AIN should be on the shortlist.
How Is It Treated?
The first and most important step? Stop the drug. Immediately.
Guidelines say: if AIN is suspected, the medication should be pulled within 24-48 hours. Delaying even a few days reduces your chance of full recovery by up to 35%. In one study, patients diagnosed within 7 days had an 80% recovery rate. Those diagnosed after 14 days? Only 45% recovered fully.
For mild cases, stopping the drug is often enough. Many patients notice improvement within 72 hours. But if kidney function is severely low-eGFR below 30-or if it keeps dropping after stopping the drug, steroids are added.
The typical steroid protocol:
- Methylprednisolone: 0.5-1 mg per kg of body weight per day for 2-4 weeks
- Then switch to prednisone and slowly taper over 6-8 weeks
There’s debate. No large randomized trials prove steroids work. But experts agree: when the kidneys are failing, waiting to see if they bounce back on their own is dangerous. Dr. Ronald J. Falk from UNC says, “Early steroids improve outcomes in severe cases.”
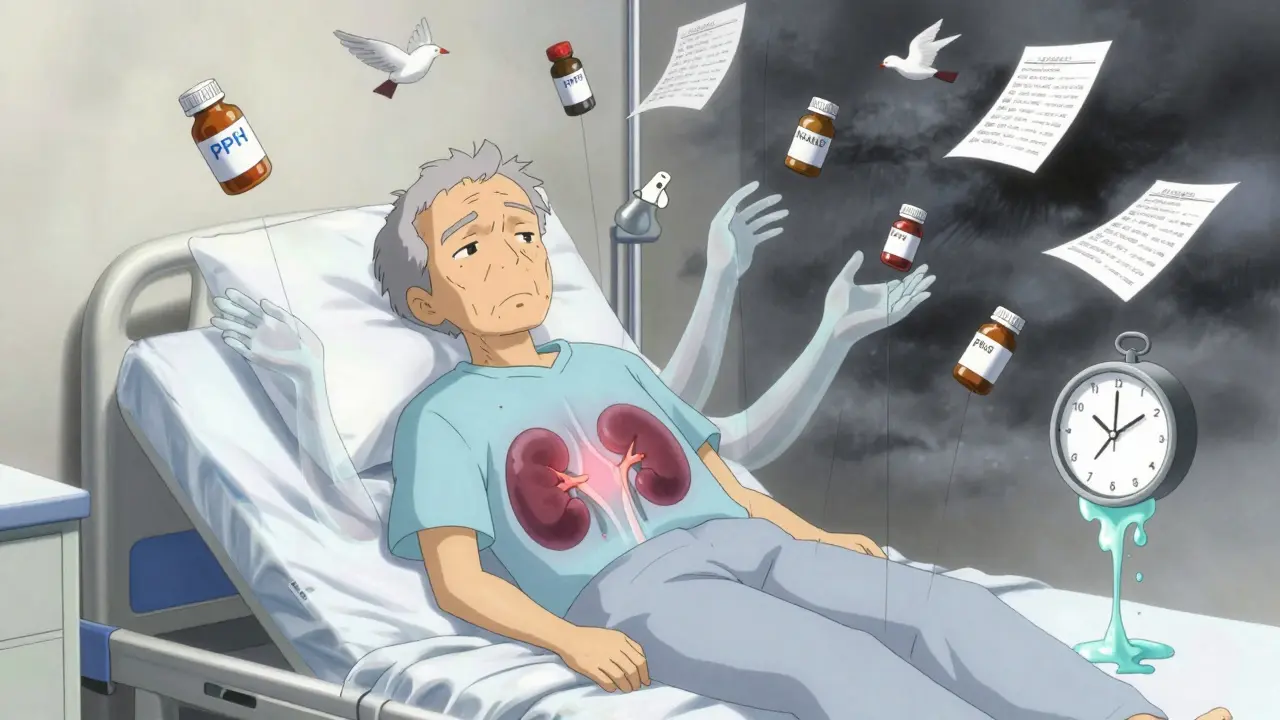
Dialysis is needed in 15-20% of cases. It’s not permanent. Most people come off it in 2-6 weeks as the kidneys heal. But not everyone recovers fully.
Recovery: What to Expect
Recovery isn’t the same for everyone. It depends on the drug, how long you had it, and how fast you acted.
- Antibiotic-induced AIN: Best prognosis. 70-80% recover full kidney function. Median recovery time: 14 days.
- NSAID-induced AIN: Worst prognosis. Only 58% recover fully. 42% go on to develop chronic kidney disease. Median recovery: 28 days.
- PPI-induced AIN: Surprisingly poor. Only 50-60% recover fully-even though the inflammation is often milder. Median recovery: 35 days.
One study followed patients for a year. Of those with AIN, 30% ended up with stage 3 or worse chronic kidney disease. That means permanent damage. No cure. Just management.
And here’s the scary part: the longer you’ve been on the drug, the worse the outcome. Someone on omeprazole for 2 years has a much higher risk of permanent damage than someone on it for 3 months.
Who’s at Highest Risk?
You’re more likely to get AIN if you:
- Are over 65
- Take 5 or more medications
- Have existing kidney problems or diabetes
- Take PPIs long-term (more than 6 months)
- Use NSAIDs daily for pain or inflammation
- Are on cancer immunotherapy drugs
And here’s something most people don’t realize: AIN is rising. Between 2010 and 2020, drug-induced cases jumped 27%. Why? PPI use exploded. In 2023, an estimated 12 out of every 100,000 people developed AIN from PPIs alone. That’s not rare. That’s a public health signal.
What Should You Do?
If you’re on a medication that could cause AIN and you notice any of these:
- Unexplained fatigue or nausea
- Less urine than usual
- Swelling in your legs or face
- A rise in creatinine on a recent blood test
Don’t wait. Don’t assume it’s “just aging.” Don’t blame your diet. Go to your doctor and say: “I’m on [drug name]. Could this be acute interstitial nephritis?”
Ask for a kidney function test (serum creatinine, eGFR). Ask if a biopsy is needed. Bring a list of every medication, supplement, and OTC drug you take-even the ones you think are harmless.
And if you’ve been on a PPI for more than a year? Talk to your doctor about whether you still need it. Most people don’t. Many can stop safely.
What’s Next?
Research is moving fast. Scientists are working on blood or urine biomarkers to replace the biopsy. CD163 is promising. Other markers are being tested. In the next 5 years, we may diagnose AIN without a needle.
But for now, the best defense is awareness. Doctors aren’t taught to think of AIN first. Patients aren’t warned. So you have to be your own advocate.
Acute interstitial nephritis isn’t a death sentence. But it’s not harmless either. It’s a silent, drug-induced injury that can turn permanent in weeks. The good news? If caught early, most people recover. The bad news? Most people aren’t caught early enough.
Know your meds. Know your kidneys. Don’t wait for a rash to appear.
Can acute interstitial nephritis be reversed?
Yes, if caught early. Stopping the triggering drug within 24-48 hours gives you the best chance. About 70-80% of patients with antibiotic-induced AIN recover full kidney function. But with NSAIDs or PPIs, recovery is slower and less complete. Delaying treatment increases the risk of permanent damage. The sooner you act, the better your outcome.
Can I take ibuprofen again after having AIN?
No. If you’ve had NSAID-induced AIN, you should avoid all NSAIDs for life. Re-exposure can cause the condition to return, often faster and more severely. Even low doses or occasional use can trigger it again. Your doctor will recommend alternatives like acetaminophen for pain, but always check first.
Do all PPIs cause kidney damage?
Not all, but all PPIs carry some risk. Omeprazole, pantoprazole, esomeprazole, lansoprazole-each has been linked to AIN. The risk increases with longer use. Most cases occur after 6-18 months of daily use. If you’ve been on a PPI for over a year, ask your doctor if you still need it. Many people can stop safely with lifestyle changes or lower-dose alternatives.
How long does it take to recover from AIN?
Recovery time depends on the drug. Antibiotic-induced AIN often improves in 14 days. NSAID-induced takes about 28 days. PPI-induced can take 35 days or longer. Full recovery means your eGFR returns to normal. But 30% of people never fully recover, even after stopping the drug. Early diagnosis is the biggest factor in how well you heal.
Can AIN lead to chronic kidney disease?
Yes. About 30% of people with AIN develop stage 3 or higher chronic kidney disease within a year. NSAID-induced cases have the highest risk-42% progress to chronic damage. PPI-induced cases are also concerning because they’re often missed until damage is already done. Once chronic kidney disease sets in, it’s irreversible. That’s why early diagnosis is critical.
Is a kidney biopsy dangerous?
It’s low-risk. The procedure takes about 30 minutes and is done with local anesthesia. You’ll need to lie still for a few hours afterward to prevent bleeding. Complications like bleeding or infection are rare-under 2%. The risk of missing AIN and letting it cause permanent kidney damage is far greater than the risk of the biopsy.
Can AIN happen without symptoms?
Yes. Some people have no symptoms at all. Their kidney damage is found only during routine blood work. That’s why regular kidney function tests are important if you’re on long-term medications like PPIs or NSAIDs. A simple creatinine test can catch early signs before you feel anything.